How to Navigate In-Home Nursing for Your Child
If you’re leaving the NICU or otherwise heading home from an extended hospital stay, then the hospital's discharge coordinators, social workers, and case managers can help you connect to in-home nursing if needed. To get more information about how to find, select, and train an in-home nurse, we interviewed Dr. Kalpashri Kesavan, medical director of the UCLA Santa Monica NICU, director of the High Risk Infant Follow-Up Clinic at Mattel Children's Hospital, and associate professor at UCLA David Geffen School of Medicine; and Undivided Navigator Heather McCullough, who is also a parent of a medically complex child.
*Note: this article pertains to home health care provided by a licensed nurse (LVN or RN), and not home care provided by non-medical caregivers.
Finding a nurse
Dr. Kesavan tells us that in-home nursing isn’t the easiest resource to secure due to resource issues in the community, but when possible, coordinators try to get families nursing care for at least part of the day — such as an eight-hour nurse in the house to help parents navigate the care of their child. Nursing care is contracted through other agencies and through insurance companies, but other resources, such as lactation services, can be sourced through the hospital’s outpatient care.
What kind of medical conditions qualify a child to receive home nursing? In general, a child who needs medical help with an essential body function should qualify for home nursing, such as:
- A child who needs help from a machine to breathe (ventilator, BiPap, or CPAP)
- A child who needs oxygen
- A child who needs a tracheostomy to breathe
- A child who uses a feeding tube (nasogastric, gastrostomy)
- A child who relies on peritoneal dialysis
- A child who needs catheterization to urinate
- A child with an ostomy
- A child who needs intravenous nutrition
- A child who has pressure sores or is at risk for pressure sores due to paralysis
- A child who has seizures that require nursing interventions
- A child with other conditions requiring complex medical interventions
Hospitals don’t always arrange for nursing at discharge, and they don’t always tell families that nursing is available. If your child has one of the conditions listed above, you can contact nursing agencies directly and ask if your child’s condition qualifies.
There are several ways to find a nursing agency. You can ask your child's doctor for a list, you can ask other families locally, or you can search online for local agencies. Contact the agencies you are interested in and discuss your child's needs to find out whether they can provide the care needed.
A different doctor may need to sign off on the nursing paperwork depending on which program pays for the nursing care. The nursing agency will ask you for a list of your child’s physicians and will send their paperwork to the correct doctor. Once you have that, find out which nursing agencies are contracted with your managed care plan and reach out to them to ask for an evaluation for EPSDT home nursing. The hospital discharge team should be equipped to assist in this process during discharge. Nursing agencies have intake coordinators who can answer questions, even if you haven’t gotten a doctor’s order yet. Most nursing agencies have a waitlist, so it’s helpful to get on the waitlist of multiple companies.
You can check out this list of resources for finding a caregiver, posting the job on the platform of your choice, or trying to recruit nurses you’ve worked with in hospitals. This is also where those support groups come in handy! Check in with your fellow medically complex families to see whether they recommend a particular nurse or organization.
The interview process
Once you’re connected to services, how do you interview nurses and cope with them in your home? It can be overwhelming to try to find the right person to care for your child, especially when your child has medical needs.
Create a list of what you're looking for in a nurse
Heather tells us that first, parents can ask the agency for a list of responsibilities that the nurses can cover — generally, any task related to the care of the child. For example, “If the child uses a cup and a plate, the nurse can wash it and put it away. They are not responsible for doing the family's dishes. If the child soils their bed linens, the nurse can do that laundry, but they are not responsible for the family's laundry. Having a list of nurse responsibilities will help set reasonable and realistic expectations.”
Tell the agency exactly what you’re looking for. For example, if your child has respiratory issues, make it clear that you don’t want a nurse who smokes. Or if your child needs to be carried throughout the day, make sure you ask for a nurse who has the ability to lift a certain weight. In this process, remember that you don’t have to say yes to the first nurse who you’re connected with. Ask questions, feel them out, and see if they are the right fit.
Tips for interviewing
Heather tells us that when interviewing nurses, you’ll want to get an idea of whether they will fit into your home. “Sometimes personalities don’t mesh well, and that's okay. You can ask the agency to send more nurses to interview if you don’t mesh with a nurse. Assuming the nurse seems to be a good fit, you’ll want to discuss experience and skills. Have they had any patients in the past with your child's diagnosis? Are they knowledgeable? I try to stay away from anyone who seems stuck in their ways. Each child is different, and a good nurse will be able to adapt to that family’s ways of doing things for that child's individual needs.”
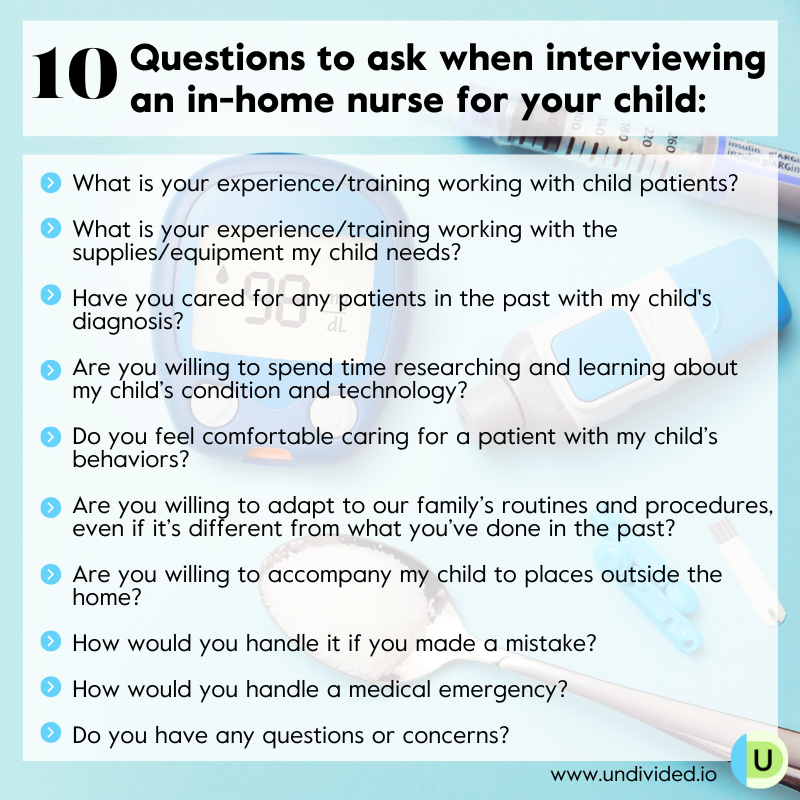
Make sure you talk about your family and how you need things done for your child. Ask them if they have questions or concerns and let them know if you have concerns. For example, “We have had nurses in the past refuse to give Timmy his bath at 8 p.m., but he needs his bath at 8 p.m. or he will not sleep well. Do you have any problems with giving him his bath at 8 p.m.?” This allows you to gauge their flexibility with your child's needs. Here are 10 questions when interviewing an in-home nurse for a child, plus 40 more you can ask a potential nurse or caregiver.
Establish a trial period
Once you’ve settled on a nurse, spend time with them and give them an “orientation” on your child. You can even prepare a booklet of important information about your child for the nurse. Of course, have a trial period and evaluate whether the nurse fits into your lifestyle and whether your child feels comfortable around them. After this trial period, you can make a final decision about sticking with the nurse or continuing your search for a better fit.
Coping with a non-family member in the home
Having a non-family member in your home daily might be initially uncomfortable. Comfort levels with having in-home providers vary with each person, so make sure to check in with yourself and your family. As Heather explains, while nurses are there in a professional capacity, they can begin to feel like part of your family.
If you have other children, for example, you may want the experience to feel comfortable, not like another version of a hospital. This is something you can express to your nurse. For example, Heather tells us: “Our nurses are free to move about the house with our child (their patient), join in family activities, sit at the dinner table with us, and truly try to fit into the home. I have a basket of our nurses’ favorite snacks for them, and if our agency doesn’t require them to wear scrubs, I let them wear whatever they are comfortable in — sweatpants, leggings, or scrubs. But some families do prefer a much more professional environment, and that's okay, too. It is truly whatever works for your family, and there can be a lot of trial and error until you find what works.”
Addressing issues
If you’ve identified concerns or worries, you can begin to come up with solutions to address them. It’s a good idea to reach out to other families who have in-home providers, either to vent or to find coping strategies that have worked for them. Our Facebook community of parents can help by offering advice and recommending blog posts, articles, or YouTube videos where others share their experiences and how they cope. There are ways to make it feel more natural while maintaining your privacy, like setting boundaries. Here are some ideas to get you started:
- Communicate which rooms are off limits.
- Provide a specific area as a “base” for the provider to work, almost like an office. This is where they will spend the majority of their time.
- Set time boundaries, such as working hours and when you need personal time for work or other responsibilities.
- Have cameras in your home when nurses will be there, for everyone’s protection. Heather shares that cameras can keep an eye out for abuse but can also help with accidents or finding information, such as when medication was given or when a certain nursing care activity took place.
Remember it's okay to find someone else if necessary
Heather adds that if a nurse makes you or your child uncomfortable, you can ask them to leave or call the agency and have them tell the nurse to leave: “This is YOUR home and YOUR child. YOU are in charge of your home and your family. It doesn't matter what it is — your personalities aren't clicking, your nurse is not understanding the care, they made a mistake that made you uncomfortable — it's okay to let the agency know and find a new nurse. You and your child need to feel comfortable in your home and with the care being provided.”
Get in-home nursing (LVN)
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor


