Out-of-Network Superbills 101
What is a superbill and when will I need one?
Typically, you’ll need to ask for a superbill from a provider who is out-of-network with your insurance plan in order to request reimbursement for some portion of these services. For example, if a therapy provider your child sees is not contracted with your insurance plan and they require payment at the time of your child’s therapy visit, you can ask for a superbill and submit it along with your claim to your insurance.
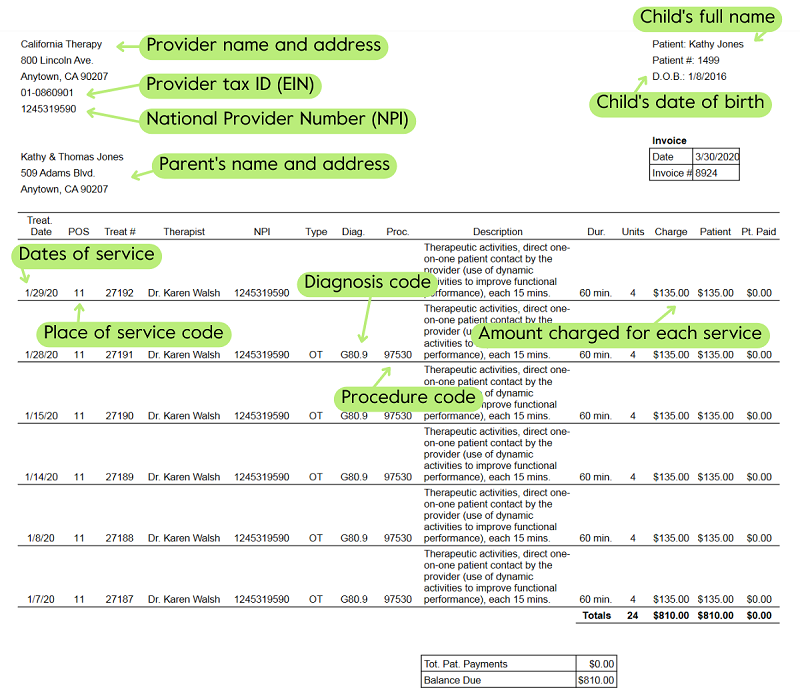
In short, a superbill is not just a paid invoice; it is a medical receipt that the health plan will accept for processing out-of-network services because it contains specific medical information, such as a billing code and diagnosis code, identifying information for the provider, and your child’s full legal name.
Undivided's Director of Health Plan Advocacy, Leslie Lobel, explains more in this clip:
What should be included in a superbill?
To make sure the reimbursement process goes smoothly, here are the elements you should expect to see on a superbill:
Child/patient:
- Child’s full name as it appears on the health plan ID card (not parent’s name) or a nickname
- Child’s home address
- Child’s date of birth
Provider:
- Provider Name
- Full Address
- Tax ID (EIN)
- NPI number (National Provider Number)
- License number
Service:
- Diagnosis and diagnosis code
- Procedure code/CPT Code/For Service Rendered — This is a five-number code that may have an alpha suffix
- Dates of service
- Place of service — This is often a two-letter code (office, home, school, clinic)
- Amount charged for each service
Here is a sample superbill with labels for each of the components above:
If you need a way to keep track of your superbills and their reimbursement status, check out this insurance spreadsheet template for Undivided members from our Director of Health Plan Advocacy services.
To learn more about submitting claims for reimbursement, how to work with your health plan, and what to do when a claim is denied, read Insurance Claim Denials and Appeals 101.
Increase out-of-network reimbursement to network level
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor


