How to Prepare for Your Child's Extended Hospital Stay
Navigating an extended hospital stay for a child can be incredibly tough for everyone: parents, caregivers, kids, siblings, family, and friends. And when your child is medically complex, it can add a whole new layer of stress and uncertainty, even if the hospital stay is planned. According to the American Academy of Pediatrics (AAP), children with medical complexity represent <1% of children in the U.S. These children “have multiple significant chronic health problems, functional limitations, high health care and resource need and/or utilization.”
Whether your child has stayed in the hospital before or you’re a new parent trying to survive your baby’s stay in the neonatal intensive care unit (NICU), we know that trying to figure out what to do, who to ask for help, and what comes next — and take care of yourself and everyone else — is exhausting! But you’re not alone. There are many things you can do to feel more in control, make the stay as comfortable as possible for you and your family, and still play an active role in your child’s care.
To help you prepare for and cope with your child’s hospital stay — and all the emotions that come along with it — we’ve enlisted the help of experts, including parents, doctors, social workers, and special education advocates. We interviewed Dr. Kalpashri Kesavan, MD, medical director of the UCLA Santa Monica NICU, director of the High Risk Infant Follow-up Clinic at Mattel Children's Hospital, and associate professor at UCLA David Geffen School of Medicine. We also spoke to several parents of medically complex children: Undivided Navigators Heather McCullough and Gabi Gangitano, who shared tips and wisdom for fellow parents, Undivided Public Benefits Specialist Lisa Concoff Kronbeck and provided insights into what public resources are available to support families raising medically complex children, and Undivided Director of Healthcare Advocacy Leslie Lobel for tips on navigating coverage under private health plans during a long hospital stay.
Note: The terms “medically fragile” and “medically complex” are often used interchangeably, though they carry different meanings and connotations. In this article, we will be using the term “medically complex” to describe children who need ongoing specialized care and to be inclusive of both conditions.
Key Takeaways
- Bring familiar items from home to help your child have a more comfortable and personalized room in the hospital.
- Explore the resources offered by the hospital to parents, such as meals, housing, laundry, social workers, Child Life specialists, case managers, and more.
- Before your child is discharged, make sure you've been trained and informed about all their equipment, supplies, medication, and follow-up care.
Prepare a hospital go-bag
Whether you’re preparing for a planned hospital stay or you have an emergency, it’s a good idea to take a hospital “go-bag” with you full of the essentials that you and your kids will need. Lisa tells us that if she is taking her child to the hospital emergency room, she brings a bag (she recommends a rolling bag with wheels) and prepares to stay overnight. “It's an easier approach, logistically, emotionally, and mentally, to go under the assumption that you're going to be admitted than to go and just hope they're going to fix it and send you home, then be disappointed, frustrated, and scared when they admit you. And that also just depends on your child. If you know that your child is likely to be admitted, go into it with that awareness.”
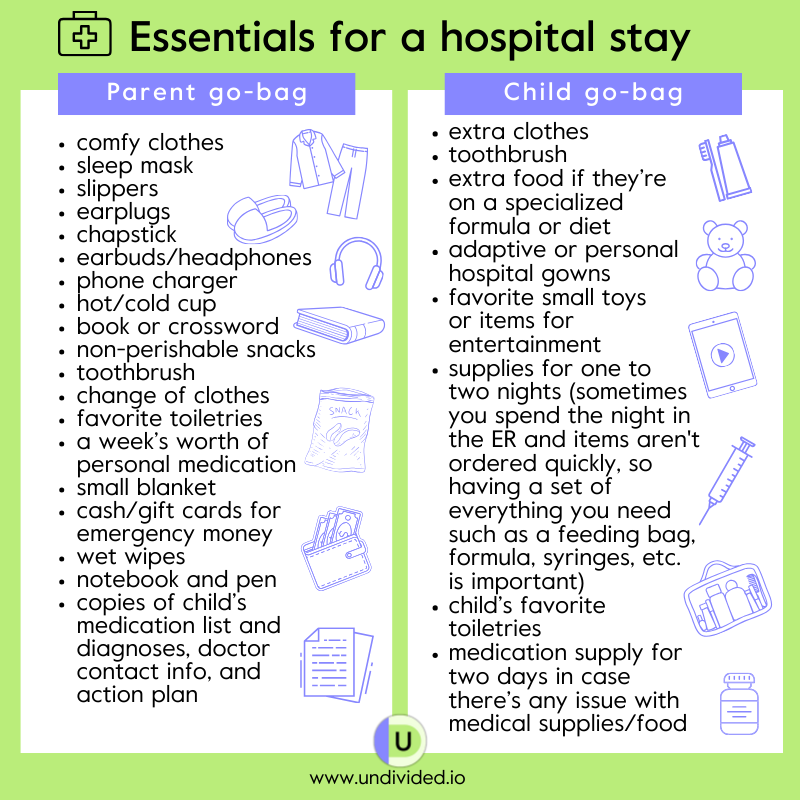
Here’s what we recommend:
Parent go-bag: comfy clothes, sleep mask, earplugs, chapstick, earbuds/headphones, phone charger, book/crossword, hot/cold cup, non-perishable snacks, toothbrush, change of clothes, favorite toiletries, a week’s worth of personal medication, small blanket, cash/gift cards for emergency money, slippers, wet wipes, notebook and pen, copies of important things like child’s medication list and diagnoses, doctor contact info, and action plan.
Child go-bag: extra clothes, toothbrush, extra food if they’re on specialized formula or diet, adaptive/personal hospital gowns, favorite small toys/items for entertainment, supplies for one to two nights (sometimes you spend the night in the ER and items aren't ordered quickly, so having a set of everything you need such as a feeding bag, formula, syringes, etc. is important), child’s favorite toiletries, and medication supply for two days in case there’s any issue with medical supplies/food.
Make the hospital stay more comfortable
If your child is going to be in the hospital for an extended period of time, creating a comfortable environment can make all the difference for you, your child, hospital staff, and visitors. There are many ways parents can do this, but first, take an inventory of things that would add warmth and comfort to your stay, regardless of whether you’re in a shared or private room. Don't hesitate to personalize with things that you and your family enjoy.
Here are some tips for making your hospital stay feel more comfortable:
Decorate
Let’s face it, hospital rooms aren’t very visually appealing, for good reason — the environment has to be safe, functional, and sterile. But you’ll be in that room for a while, so having familiar decorations and objects can help. Here are some ideas for making the room feel more like home:
- Make sure everyone who walks into the room knows your child’s name. Here is a Hospital About Me printable that you can fill in and put up in the room.
- Decorate with seasonal decorations to make the room feel festive and fun (dollar stores have some great seasonal options!). Put up family photos around the room. Having objects that feel familiar can also help.
- Bring blankets and pillows from home so that the bed feels like their own. Whether this is allowed depends on the facility and their policies as well as the stability of your child, so check with the hospital first. In addition, check with the hospital laundry facilities to find the best time to wash the bedding.
- Bring in a foam topper to put on the pullout bed, if the hospital allows. It gives a soft, more homelike place to sit with your child other than their hospital bed (make sure to check with staff first). Some hospitals may even allow toppers for the child’s bed. We talked to some parents who have even brought in an air mattress to put on top of their hospital bed for a child with limited mobility, which the doctor can order for your child to use.
- Remember, it has to feel like home for you as well, so bring your own pillows, blankets, slippers, sweatpants, pajamas, beauty products, bathrobes, eye masks, teacups, headphones, phone chargers, etc. — or, as Heather says, all the essentials “that you would want to just drown out the fact that you're in a hospital periodically… If you were camping, what would you want to bring? That's what I bring.”
- Personalize your child’s room. You can even bring a favorite storybook, notebook, scrapbook, or something for the medical team members or visitors to sign with well wishes and messages for the future. That’s what Lisa did: “We had coloring books and we had crayons, and anyone who came to visit would color a page and tape it up on the wall. So we had a whole wall of colored stuff. It's just anything that you can do to personalize the room and make it a comfortable, welcoming space. It just makes it feel less hospital-y.”
Make it fun and engaging
While the hospital has to be a sterile environment, Lisa reminds parents to make sure it doesn't feel like an emotionally sterile environment: “I don't mean in terms of germs but in the feeling of it. It's nice when there are things that are stimulating for them to look at and engage with. And if they're in the hospital for a long time, they're going to be having to do some of their early development there.”
Some things you can bring include forms of entertainment such as tablets, coloring books, or whatever your child’s favorite things are. Child life specialists can help with this by bringing crafting supplies, toys, and other things for your kids that can help them feel like they’re at home (more on Child Life later!).
Play music
Another way to bring comfort to the hospital is with music. For Leslie, playing music in her child’s room was the number one thing she did for her sanity. She believes that it also improved the experience of everyone who entered the room. “I had classical music on around the clock,” she says. “Everyone who walked in the room stopped for a minute; it changed me, it changed the environment. It was a very small thing, but it spoke to medical professionals as well as the people who were cleaning the room. There was something different about our room because it had this classical music on, and it was a way for me to tell all the doctors, nurses, specialists, and respiratory therapists that something different was happening in this room, and that we were creating sort of an environment.” Even if you don’t have your own room and are in the NICU, you can play music, such as lullabies, for your baby.
The Child Life Program
There is a ton of support you can get at the hospital, and Child Life is an important part of this. Most hospitals have child life specialists who are educated and clinically trained to work with doctors, nurses, and you and your child throughout your child’s hospital stay. They provide emotional support for parents and kiddos to help reduce all the anxiety of being in a hospital. They can bring things like toys and coloring books, as well as music and art therapists, service dogs, and more.
Heather tells us that Child Life is a huge resource that she recommends for everyone facing a 24-hour or extended hospital stay. “Their job is to come in and just make your child feel more like a child. They're there to help [your child] process what's going on. They can help them understand all the testing, the medical words they're seeing, the equipment being used, and the jobs of everyone in the hospital. They can also offer enrichment to the child while they're in the hospital. They can bring them toys, games, activities, and they also put on little events. If your child is able to attend those events, child life specialists can be very helpful in creating better morale and boosting spirits. That's their job, and they're all fabulous about it.”
The hospital should have a Child Life Specialist to provide some support in the context of helping your child cope with being in the hospital, so when you’re admitted make sure to ask about it. Read more in our article Child Life Specialists 101.
Ease MRI anxiety: ask for a LEGO® MRI Scanner
MRI scans can be scary for anyone, let alone children. If your child is scheduled for an MRI, here’s something that might help calm those nerves — LEGO! LEGO® MRI Scanner sets are being donated to hospitals around the world to help kids understand what happens during an MRI in a playful, hands-on way. The idea is simple but powerful: when kids can see and play through what’s coming, it helps take away a lot of the fear of the unknown.
According to a 2024–2025 LEGO Group survey of hundreds of medical professionals who’ve used the set, 96% said it helps reduce children’s anxiety, and nearly half said it even helps reduce the need for sedation or anesthesia.
The set isn’t available for purchase — it’s donated exclusively to hospitals — so parents need to work through the hospital, usually Child Life Specialists, radiology managers, volunteer services, etc. Ask your child’s care team whether the hospital already has the MRI set. If the hospital doesn’t have one, ask Child Life or the radiology manager whether they can request one through the hospital’s volunteer services, patient-experience team, or partnerships team (these groups request donated items from companies and charities).
Daily care for kids and parents
Parenting in the hospital can take us out of our comfort zone, literally. We may not have access to all the daily care activities we would like to do with and for our kids, but it’s important to continue parenting “as usual” as much as we can to preserve some sense of familiarity and consistency. For example, if you read your child a bedtime story every night, continue doing so. While some changes are to be expected, you can continue to be involved in your child’s daily care. Here are some ways to do so:
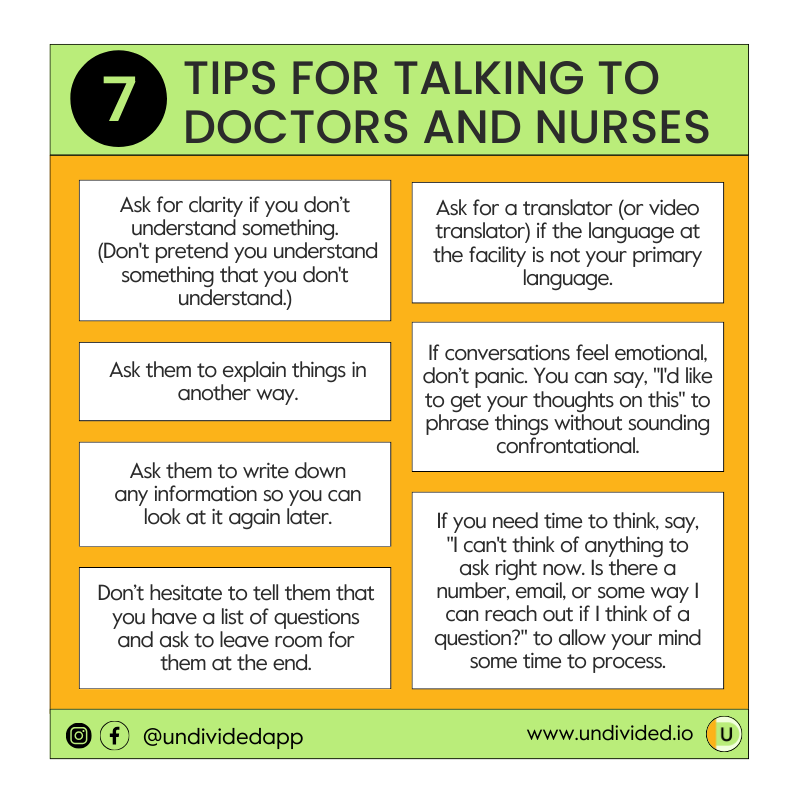
Ask questions and take notes
It’s easy to feel scared or intimidated when surrounded by doctors, nurses, and loud machines. But you’re an important member of your child’s team and have a right to be informed of what’s going on. As Leslie tells us, “Make a list of all the questions you have. Don't rely on your memory. When the doctor comes in and there’s a limited amount of time, have your questions ready and write down what they say. If you know that the doctor is coming at a certain time, that's a really great time for both parents to be there, or for a parent and another trusted family member to be there. If you know there's an important specialist coming, that's a great time for more than one person to be listening, especially if one of them is exhausted. You can ask people to write something down, you can take notes, or you can ask the doctor or the nurse to put it in writing for you — ‘Can you write that down so I can look at it again?’ Because sometimes you can't remember what they said.”
Be present for your child’s hospital rounds
Being present for your child’s hospital rounds is a great way to be involved in your child’s care. When you get admitted or when your baby is born, you can ask what time rounds are and have the nurse tell the floor team that you want to be a part of the rounds. Staff are usually more than happy to accommodate parents during rounds. If you do get pushback, that is a red flag and something to let your social worker, nurse, or doctor know about.
Ask for consultations (and anything else you need)
Although your child may be in the hospital for one reason, there may be other areas of need you’ll want to address as well, such as nutrition, occupational therapy, and physical therapy. You can always ask for a consultation with one of those departments if needed, as well as ask for other items you need, such as an air mattress, moisturizer, washcloths, additional towels, diapers, tissues, wipes, etc.
Don’t forget to eat
It sounds obvious, but when your child is in the hospital, eating is probably the last thing on your mind. How long the stay will be, what treatment or medication will be given, what all the new words mean — yes. Food? No. But it’s important to remember that how we show up for our kids is directly related to how we show up for ourselves, and taking care of our bodies is a huge part of that.
When it comes to food, that’s a bit of a complex issue because every hospital is so different. Talking to the social worker or a hospital support group can help you figure out your options and what kinds of resources your hospital has. As Heather explains, sometimes hospitals will have meal trays for parents, which can take a load off your mind. But if the hospital doesn’t offer that, you have to figure out food yourself. Heather and Lisa offer some of their food-related tips:
- Keep some kind of nonperishable food in your hospital go-bag so you have something to tide you over until you figure out what to eat.
- Take advantage of DoorDash, Uber Eats, Postmates, and other food delivery apps. You can even ask family and friends for gift cards to these services.
- Grab food at the cafeteria, vending machines, or places that are close or within walking distance.
- Sometimes hospitals have a family resource center with donated items they can give you, such as coffee or granola bars. Heather’s former hospital had a Subway in it that would donate sandwiches to the family resource center, so families could get a sandwich every day.
- Ask a friend to create a food train where people pick a day to bring you food. If you have a significant other, you can also ask a friend to help them, especially if you have other kids at home and no time to cook or shop.
- If you're nursing or pumping, some hospitals may have nursing mom food trays, so that’s another thing to ask the hospital about. You can also check out a Ronald McDonald House, which also offers meals and snacks (you can get a day pass and check them out, even if you aren't staying in one).
- Drink plenty of water. It’s easy to get dehydrated with dry hospital air.
Don’t forget to sleep
Sleep is another major area of self-care and one where you might have a lot of questions. Can I sleep in the same room as my child every night? How many people can stay overnight? What happens in the NICU? Should we stay every night? Sleeping arrangements typically depend on the hospital and what level of care your child needs. For example, Heather explains that there's usually no bedside sleeping in the NICU, so parents may need to reach out to Ronald McDonald House (more on this later) or find an inexpensive hotel or someone to stay with nearby (if they’re not local). Social workers are a good place to start, and then you can talk to other families. Socializing with other families in the family lounges is a great way to find resources. Note: check with your insurance about sleeping assistance. Sometimes insurance or Medicaid will cover the cost of a hotel room in part or in full if there is no bedside accommodations for a parent.
Sometimes parents will be able to room in with their child, but the hospital may only have room for one parent, so you’ll need to figure out how to navigate that as well as how to support your other kids. Some hospitals have beds they can wheel in, which can accommodate both parents staying the night. They may also have parent rooms, but they’re not usually not the best long-term option if your child is in the hospital for a month or more. But parent rooms do have resources, like a shower, so that you can go and just take a break and step away. It’s very much hospital dependent, so ask the hospital what kind of resources they have available.
Bedside sleeping is an important aspect of staying at the hospital because you never know what your child or the nurses/doctors are going to need in the middle of the night. Plus, it may help with your mental health to be there to help your child in case they need you.
That being said, mental health also means taking time for yourself. As Heather states, “You do need to take time for your own mental health and take a break, get out, breathe, and recharge. And you should never feel guilty for doing that. They are in hospital, they do have people caring for them. They should be safe for you to be able to go take a minute, breathe, and take a nap or a shower, and you should not beat yourself up for it. You investing in yourself is investing in them. The judgment of other parents who are not in that situation and have never been in that situation are the ones who I think judge the hardest. That's where I felt the judgment from — other families who've never been in this position — ’I would never leave my kid in the hospital overnight.’ Well, when you've been there for six months, you might think differently. It's important to take time for yourself.”
While it can be hard to leave your child alone in the hospital, after some time has passed and you and your child are familiar with the routine, nurses, and other staff, it will be easier to leave them overnight. Leslie tells us that she and her husband stayed at the hospital until 9 p.m. to make sure that the nurse changeover was effective, then went home and slept. “We came back in the morning because it was essential not only to us, but it was actually better for our daughter's care because she had a non-exhausted parent who was able to listen to what the doctor said and make an informed decision. That was really hard to do. Our fear was that the nurses were going to think we didn't care about our child. It is really hard to leave, but it's really important that you sleep. It's not negotiable.”
Ask about Ronald McDonald houses
If your child is staying at a hospital far away from home, housing is going to be on your mind. Ronald McDonald houses can be a great resource for families who don’t have relatives to stay with and don’t want to or can’t afford to stay long-term in a hotel. The Ronald McDonald House programs “are a home away from home that provide comfort, support and resources to families who travel far from home for the medical care their child needs.” How can you stay in one? Contact your social worker or the social service department at the hospital where your child will receive treatment, and they will place your name on the waiting list. Families either stay at no cost or are asked to make a donation up to $25 per day, depending on the facility. Stays can last as long as several months and sometimes extend to a year or more.
There can be a waitlist, so it's not always a guaranteed option, but it's worth looking into. Different hospitals may also have their own local housing options, so ask your social worker for resources.
Do laundry
Some hospitals have laundry facilities for families to do laundry. Check with the hospital to see if this is available. Bring a bag or even an extra pillowcase that can serve as a laundry bag. (Dissolvable laundry soap sheets make for a lightweight space-saving option in your go-bag.)
Find a community
Having a support system and community of parents who have been where you’ve been and have experienced the highs, lows, and everything in between of having a medically complex child in the hospital is essential. There’s only so much we can do on our own — reaching out to support groups and communities can help us find resources, share our fears, and get tips and advice we can’t get elsewhere. Hospitals usually have a support group, so make sure you join and ask other parents what's available in the area and what resource options you have. “The parents, they've been there, they've been in the trenches, and so they will share the resources and tips with you,” Heather says.
Heather tells parents that networking is key. “I learned more from other parents to start off with than I did from the hospital. The hospital was great at keeping my kid alive, but the other parents were great at helping me to understand what I needed to be doing, how I needed to be asking questions, and [how to find] resources (like pediatricians that were capable). I can't just go into an average Facebook group for moms and ask for a pediatrician recommendation. I need to ask people who have kids like mine.”
Leslie agrees, sharing that it’s important to reach out to other parents for advice, tips, and ideas. “Are you in any kind of diagnosis-specific support group or a community around the experience where you can ask other parents, ‘What did you do when your child was in a body cast? What did you do when your child was transitioning to feeding? What do you do when the oxygen masks irritate the face? What are the best products? What are the best workarounds?’ It's like going online to look for a recipe: Which brownie should I bake? Oh, a bunch of people are putting salt in their brownies. These people are putting caramel in theirs, these people are using butter. It's the same thing. What's the recipe to take care of a body cast? What's the recipe to keep my child from having skin breakdown? Because they're going to be in a hospital bed for a while.”
NICU TIP: you can still be a parent, even in the NICU
As a parent, you’re a partner in your child's care even when they are newborns. It may feel scary to get hands-on with a baby who is tiny and hooked up to monitors, but remember, you have nurses to help you along the way and make sure you’re trained and comfortable caring for your baby.
Here are a few things you can do to bond with your baby in the NICU:
- Participate in your baby’s care by doing things like changing your baby’s diaper or helping with feeding and bathing.
- When possible, hold your baby, including for skin-to-skin bonding.
- Hold your baby’s hand or place your hand on their back.
- Talk to your baby, and read or sing to them.
While NICU nurses can be protective of the babies in their care, you can ask to be involved. This will help when you transition home. It’s also great for your mental health as a parent, as well as for your baby, like Heather says, “to know she wasn't alone and to be able to feel that human touch. When I was able to hold her, I felt like there was already a connection, even though she had never truly met me because she was asleep the whole time. I think I was familiar to her, and I think that was important to do for both of us.”

Dr. Kesavan explains more of how parents can be involved:
It’s also important to support your own needs during this time. Speaking specifically about the NICU, Heather tells us that the NICU is “just a different world.” She continues, “Every kid is so different, their needs are so different, their level of fragility is different. It's crazy to look at all the different babies, you know, the different sizes and how sick they are. The amount of machines that you may see, the isolettes, the tiny babies, the staff. You may hear alarms going off all the time. It's very overwhelming as a parent, and so you have to take time for yourself, step away, breathe, go eat something, take a shower, take a nap. I mean, a lot of times a nap will change so much about your day. You could be having the worst day — you could be on the brink of a breakdown because your baby had a bad day — and if you get a nap in, it just recharges you.”
Celebrate the milestones, especially in the NICU
If you’re expecting an extended stay at the hospital, especially in the NICU, your child will probably have many firsts while you’re there. Just because they happen at a hospital doesn’t make them any less important. Remember to celebrate as many milestones as you want. Here are a few things to do while in the NICU:
- Get handprints and footprints, which can be done at discharge for a short hospital stay, but you might want to do it early on if you’re anticipating a long stay.
- Get newborn pics while inpatient if you’re expecting an extended stay. You can bring in a photographer, or sometimes the hospital will have a photographer.
- Celebrate every milestone! You can use these NICU milestone cards for every tiny step forward by placing a card next to your baby and snapping a photo. The cards include phrases such as: “I’m going home today” and “I’m breathing on my own today.”
- Take a first family photo with baby and parents.
- If you have other children, find a way for them to be involved with your NICU baby. Younger siblings may not be allowed to visit in-person during cold and flu season, but you can set up a video chat so that siblings can feel connected to your newborn.
Prioritize your mental health
Having a child in the hospital is downright stressful, whether you have a baby or a teenager. There’s a lot to deal with logistically and emotionally, so the whole experience is often draining. Every parent and expert we’ve spoken to has emphasized the importance of taking care of yourself during an extended hospital stay, whether that’s eating right, taking a nap, or asking for help.
- Take breaks. It’s hard for any parent to leave their child at the hospital. The guilt and worry can be all-consuming. But you can’t care for your child if you don’t care for yourself. Leslie shares that if your child has been in the hospital for a very long time and the routine is known, use your time efficiently. “It may not be possible, either for financial or mental health reasons, to be at the hospital around the clock. And it depends on the age of the child. I'm not saying that you should leave a two-year-old alone in a hospital room all day. But my husband and I took turns.”
- Ask for help. Leslie tells parents to ask for help from friends and family as much as possible because even if you are in the hospital, your home doesn't stop. “If the situation at the hospital is not 100% resolved, there's ongoing care that needs to happen at home…. There are all kinds of tasks. Don't be afraid to ask people to help out with carpooling. Maybe someone could commit to come and put your garbage cans out once a week. People want to do something and they don't know what to do.” She also adds that if people are asking how they can help, ask them if they can stay at the hospital with your child for a few hours, just so you can go home, take a shower, and take a nap.
Tips for advocating for your child with hospital staff
Regardless of whether your child’s hospital stay is anticipated or totally unexpected, there will be a lot to absorb and learn. Knowing the ins and outs of navigating the hospital can help your experience be a bit less stressful.
Get a deeper dive on this in our article Tips for Advocating for Your Child with Hospital Staff.
Finding a support team at the hospital is one of the best things you can do for you and your child, especially amidst all the changes happening. That’s where social workers and case managers come in — to help you cope with everything associated with your child’s hospital stay. Social workers can help with coordinating care, connecting to resources, communicating with the medical team, finding emotional support, and navigating the medical systems.
Heather tells us that hospitals often have a variety of resources for families, depending on the situation. “For long admissions, sometimes families have a hard time with meals, with parking (if your hospital charges for parking), with lodging. [Social workers] can potentially have meal vouchers or hospital discount rates for local hotels. And they can help you get into places like Ronald McDonald House or other charities that may have lodging available for families for long hospital stays. There are other resources too, but each hospital is just so different. You can't say that all hospitals have the same resources; they all have their own types of resources based on the area they're in and what they feel is helpful to families, and what they're seeing most families need or [don’t] need.”
Social workers, case managers, and patient advocates
For resources, Heather tells us that social workers, depending on their background, are there to guide you through that hospital. According to CHLA, “The social work team’s goal is to support every family and make sure they have what they need while a child is hospitalized. [They] work with you to determine your needs and the best way to address them.” For example, connecting families with hospital and community resources, discharge planning, counseling and mental health support, finding support groups, helping families communicate with doctors and nurses, and more.
Patient advocates, Heather adds, are usually from a different department than social work and are there to help you if you have a problem with communication or safety. They’re focused on promoting your rights and making sure your voice is heard when problems or difficulties arise. “They're there to help you be heard. I have had to call patient advocacy many times to have situations resolved, and I've never had a bad experience with them. They've always been very helpful, at the very least drawing attention to the problem. Let's say the team isn't necessarily taking me seriously; having that patient advocate shine a spotlight and say, ‘No, this is a serious issue. We do need to address it’ is super helpful.” Some patient advocates are directly employed by the hospital, while others may work through a nonprofit organization, such as the Patient Advocate Foundation, that you can hire privately. One type of a patient advocate is the hospital ombudsman, who can help with more serious concerns and conflicts. Every hospital will be different in what resources they offer, so ask your social worker to connect you with the right person.
Leslie explains that case managers, who are usually hospital nurses, are also very helpful if your child is in the hospital for a long time. According to UCLA Health, “The clinical case managers ensure that the care [their] patients receive is coordinated, safe, timely, and effective, efficient, equitable and patient centered.” Leslie says, “You may want to call the plan and try to get a case manager assigned. Case management can be a helpful thing or a completely unhelpful thing. It depends on a few factors, including what nurse you get assigned to. So the upside is, they're actually nurses. Sometimes they're just shills for the health plan and they're just trying to protect the health plan. But sometimes they can actually help you think about benefits you might have that you're not using, and maybe even sometimes interface with the billing department at the hospital.”
You can also ask for things such as a chaplain or mental health services, like a marriage and family therapist, or different food options (kosher, vegetarian, etc.), Leslie tells us.
NICU TIP: lean on your NICU team for support (that’s what they’re there for)
If your child is in the NICU, you will meet the NICU team. Dr. Kalpashri Kesavan, MD, tells us that the primary team parents will be interacting the most with is the neonatologist and the doctors who are in that team — usually a group of fellows, residents, and others, especially if you’re in an academic center like UCLA. However, your point person will be the nurse who gets assigned to your baby. “When we anticipate a longer course in the NICU, and in more medically complex cases, we do have a primary care nurse assigned to the family. So they are able to have this nice personal interaction with them. But in addition to the doctor-nurse team that we have, we also have ancillary services because we can't do without them. We have our respiratory therapist, occupational therapist, and physical therapist. We have our social worker, case manager, and discharge coordinator. So it's a pretty big multidisciplinary team that is caring for this very young, small baby.”
Dr. Kesavan tells us that while the nurse is the point person for parents regarding everything happening day to day, such as the baby’s progress or challenges, “there's a social worker who periodically touches base with them so they can help them according to their needs or if there are other resources that they need to be plugged into. For instance, if they need therapy or family development care and other things, it's really our social worker who helps them get into those programs.”
Lisa shares one experience with her NICU social worker who helped her as she coped with her daughter’s stay: “One of the best things that our NICU social worker told us was that the NICU is often three steps forward, two steps back. And don't get discouraged if your child regresses because that's the natural progression of things in the NICU. It's not always progress. And that's just one of the things to remember when your kiddo is in the hospital. Even if it's not the NICU, even if it's a long hospital stay — it's not a straight line.”
If you have concerns, you can reach out to the ombudsman or patient advocate, but Dr. Kesavan says that usually the NICU team will take on the concerns with a social worker being the liaison, “so we can help meet the family where they are and help understand their goals of care for their baby and sort of work towards that goal.”
NICU TIP: secure breastfeeding equipment through private insurance
Resources such as breastfeeding equipment should come from the hospital through private insurance. “If your child has a feeding tube, then you may be able to get a rental of a hospital-grade pump covered under your insurance. They'll give you a manual breast pump and sometimes even a battery-operated breast pump as part of your insurance coverage, but if you have a child who's tube-fed and they're consuming breast milk, you can sometimes get a hospital-grade pump rental covered as a medical necessity because the child can't nurse.”
Funding extended hospital stays
Trying to navigate funding, insurance, and public benefits can be overwhelming, especially when you’re first admitted to the hospital. Should the hospital be guiding you through all this? In theory, yes, but they might not always have that information or have much direct experience with the resources or systems you need to know.
Hospitals will be in-network for most plans, and with their own billing departments, they will be adept at connecting with your health plan and getting everything started when you’re admitted. Leslie explains that in-hospital authorizations to stay overnight in the hospital are given in two- or three-day increments. Usually the billing department will be on top of that, but you can always reach out to check that everything is going okay or let them know if there is a problem.
If your child is in the hospital for a long time, you will likely soon reach the out-of-pocket maximum for your primary health plan, but you will want to be aware of what your plan has as the coverage for the benefit for hospital stay. They'll probably keep you authorized up to a certain point, but you should know what your percentage is past that authorization. That's where you want to make sure you have a secondary payer, whether a spouse’s insurance or Medicaid. If the hospital you're in accepts Medicaid, they will bill the primary and they'll bill your child's Medicaid. If you don't have Medicaid or a secondary plan, you'll have a dollar amount responsibility. That's where you're going to want to know how long you'll have that percentage and where you are in your out-of-pocket maximum for the year.
NICU TIP: consider getting your baby onto Medicaid through SSI
If you’re in the NICU for months, a big challenge will be getting your baby onto Medicaid if they're not already on it. One avenue that you might consider is getting your baby onto SSI, which can be a foot in the door to Medicaid, at least until they get discharged. As Lisa explains, if you have a baby who meets certain criteria, such as being born before a certain period of time or under a certain birth weight, they'll automatically be accepted for SSI. You can provide that documentation to SSI, and they can get your baby covered under Medicaid.
Once you’re out of the hospital and you no longer qualify for Medicaid because of household income, you can look to a waiver program for kids with disabilities.
What to know before heading home
Heading home can be an equally joyful and terrifying experience for families. It’s a relief to be able to take your child home, but it also comes with fear around next steps. Here is advice from our team of experts about what to do and know while preparing for discharge:
Know when discharge is happening and what it will look like
Try to discuss everything with the discharge coordinator and potentially the case manager at your health plan — in advance if you can. Start asking doctors and nurses to connect you with discharge planning early so that you can have everything arranged for when you return home. You can reach out to a nurse with whom you have a good relationship and ask what they would recommend you do and plan for discharge. Try not to get discouraged if discharge doesn’t happen the day you expected it.
Logistics are the big thing here. Leslie tells us, “Everybody wants to get out of the hospital. Everybody's question is, ‘Thank you very much, when can I go home?’ What I would encourage people to do — while focusing on the fact that they can't wait to get out of the hospital and back to normal routine — [is to think about] what they want to have in place to support the most normal routine they can have when they arrive home.”
NICU TIP: Dr. Kesavan explains more about what discharge from the NICU looks like:
Organize supplies and equipment you will need at home
Do you need equipment to go home with, such as oxygen support, medical food, diapers, or adaptive equipment for your home? If any of those items, either rentals or purchases, need pre-authorization, ask for those in advance.
- Make a list of all of the equipment and supplies you need and make sure the hospital tells you how often you need to reorder, provides you with a list of phone numbers where you need to call to reorder, tells you if there will be any copays, and tells you how often you can order each set. Some things you can order only every 30 days, while others have to be replaced every six months or every year. You might have to call your plan or look online to find out who is the in-network, contracted provider of durable medical equipment. If you have a good discharge coordinator, they may give you a list of places.
- Make sure supplies and equipment are delivered before you get home. Call and set up an account with the durable medical equipment company, and preorder so that an order can be waiting on your doorstep or delivered the day you arrive home. That should be coordinated by whoever's in charge of discharge at the hospital. If the day of discharge changes for whatever reason, make sure that all of the deliveries get changed too.
- Make sure you have all the supplies you’ll need (and extras!). For example, if you have a g-tube but you don't have extensions or feedbags or formula, the pump isn't going to do a whole lot of good. Check that you have extras of what you need, such as an extra kit for a g-tube, because if that g-tube comes out, you want to be prepared and trained in replacing it and not have to rush to the hospital.
- Ask the hospital staff for help. When you’re leaving, you will get a discharge summary with prescriptions of medicines you need to get. If you know you don’t have the bandwidth to go to the pharmacy, you could convey that to the doctor or the nurse and ask them to help you put in an order so that those medications can be delivered. Don’t be afraid to ask the nurses, “Is there anything you can think of that I might want to prepare for at home? What could I do?”
Get trained on equipment (and everything else!)
Leaving the hospital can feel like a scary leap, especially when you’re going home with equipment, machines, oxygen, and more. Making sure you’re getting trained in everything you need will set you up for a smoother transition home.
Training on equipment should come from the DME providers, depending on what it is. If you're getting a wheelchair, feeding pump, or CPAP mask, for example, the people providing the equipment should train you on it. For example, when they mail you a wheelchair, usually a wheelchair technician will come in and set it up for you. Other things, like a feeding pump, are better to be trained on in the hospital. For that, delivery can be to the hospital before you leave, so that the nurses and/or doctors can train you on it (if the person who's delivering it can't).
Heather adds that hospitals also make you room-in, which means you’re restricted to the room with your child for 24-48 hrs and you pretend to be home. “You provide all the care and do everything on your own to give you practice and make sure you know how to do it all before you can leave. It's a big deal,” she says. During a room-in, you’ll have to coordinate food, whether that’s ordering a food tray, using food delivery, or having someone bring you food. “If you have two caregivers rooming in, most hospitals will allow the caregivers to take breaks individually. One could get food, take a walk, do laundry, etc.,” Heather adds. “But It's a practice run for home, and just like at home, you wouldn't leave your child alone. As you get close to discharge, you should ask your team what their rooming-in for home preparation looks like so that they can prepare you and you can make arrangements (such as taking time off of work if you need to).”
For car seats, while you can book an appointment at your CHP/police station (hey usually have free car seat installation services where you can book an appointment, bring the car seat, and they'll set it up for you), Heather tells us that setting up a carseat looks very different for medically complex children and that families should talk to their team about it when they start talking about discharge:
“There is a very special car seat test that has to be done on medically [complex] kids. [During the test] they put the baby in your car seat and put an oxygen monitor on them. The baby must hold their O2 saturation for a certain amount of time (usually 2/3 the time it takes for you to drive home). If the baby cannot hold their o2 SATS, they don't get discharged. My daughter was given the wrong test — they had us show them that we had a car seat and knew how to buckle and unbuckle it — and I didn't know there was a different test for medically [complex] kids. We were life flighted back to the hospital as a result. It's very important that families know that there is a special car seat test that should be done by the hospital for medically [complex] babies and kids.”
Dr. Kesavan tells us that for parents leaving the NICU (although this can apply to all areas of the hospital), the goal is “to make sure that everything from the basic care for the baby, to safe sleep, to whatever complexities the baby may have, to the medications, equipment, oxygen, feeding tubes that they may have to go home with, that everything happens in the NICU and they are comfortable doing it before they go.” This would generally be something that the discharge planners start thinking about very early on, and when you get closer to discharge, the team makes sure that the equipment has been delivered to your home and that you are familiar with using it.
“Even giving medication like multivitamins and iron, we teach them because babies don't take medicines easily and well. So we want to show them how to use the feeding pump, for instance, or how to use the oxygen machine. We also have reps from these companies that are providing the equipment come and teach them, along with the nurse.” She adds that it could be a long process, sometimes weeks, to set parents up to be ready to transition out of the hospital. She adds that, “In addition to that, our discharge coordinators actually reach out to the families after discharge, a week or two, just to make sure it's all going okay and they're not facing any challenges with that as well.”
Know who’s in charge of what
While your child’s pediatrician will handle the everyday things, specialists may manage other items. Depending on a child’s specific needs, things that you're having ordered may need to be managed by different specialists on their care team. For example, oxygen may be managed by a pulmonologist while feeding supplies may be managed by a GI doctor.
Set up follow-up visits
Making sure you know what the plan is for follow-up visits is key in easing into home life. You want to know who to call and when your next appointment is going to be. If you have a pediatrician you love, great! However, Heather adds that going to a complex care clinic (if possible) will be great for pediatric care versus just going to a general pediatrician’s office. Why? They’re familiar with writing orders for complex medical things that you will need, and they’re aware of how fragile your child is and won’t overlook things. “You definitely need to make sure your pediatrician is comfortable handling your child, is aware of what's going on, and has the ability to manage them,” Heather says. “My daughter was turned down by different pediatricians when she came home. They were like, ‘Nope, not doing that. We don't know how to order any of that stuff, not doing it.’ So we do use a complex care pediatrician now. But there was a point when we used my other two kids’ pediatrician because he was competent and he was comfortable, and he had done this stuff in the past. So it just depends upon your situation and what you have access to.”
What exactly is complex care? Heather tells us complex care pediatricians work in complex care clinics, like this one at Stanford, and your discharge coordinator can help you connect with one. You can bring it up during your child’s hospital rounds and ask for them to set you up with complex care (sometimes they'll just need to send over a referral), and/or you can look on your hospital's website to see if they have a complex care clinic. “They are considered a specialty which is why you'll need a referral a lot of times. They take care of children who are medically complex, and sometimes their siblings too. These clinics have social workers, care coordinators, case management, dieticians, etc., and they are very familiar with filing paperwork like orders for equipment, supplies, prior authorizations, and sending referrals. They're familiar with the lingo and terminology used with medically complex kids and are familiar with their unique needs. Oftentimes, they act as an in-between place when your child is sick and you don't necessarily want to go directly to the ER. The complex care clinics can function like an urgent care in that they can perform care that a typical pediatricians office can't. They can also directly admit patients which is super helpful when you have an immunocompromised kiddo, for instance.”
NICU TIP: continue participating in NICU care, even when you go home
If your baby is in the NICU but you are discharged, you can continue to participate in your baby’s care depending on how you’re feeling, physically and mentally. “That's the first thing they want to make sure they are doing — self-care,” Dr. Kesavan says. “Before they start being able to do more for their baby, we do actually encourage family-centered rounds; we like them to be participating in rounds. Sometimes we have them call in while we're rounding on their baby. Sometimes they're there physically a few weeks down the line when they do feel better and are able to join rounds and don't have other commitments. We actually ask for their input — if things are going the way they are hoping or expecting. Or if we're having challenges, we let them know why we're having challenges… We start with having them get included in the care of their baby and the sort of the plans we are making for the baby.”
Here’s a tip sheet of the most essential questions parents should ask before leaving the hospital:
- When is discharge happening?
- What do I want the discharge day to be like and who do I want there with me?
- Are there any videos, classes, books, or apps that can help me learn how to take care of my child at home?
- How can I prepare to arrive home?
- Is my home set up, organized, and ready for my child to arrive?
- What do I want to have in place to support me when I arrive home?
- What equipment, food, and prescriptions will my child need at home?
- Is everything set up to deliver by the time I arrive home?
- How often do I need to reorder equipment? Who do I reach out to order?
- Which provider is in charge of which supply, need, or prescription?
- Do I have extras (at least a month’s worth) of everything I will need?
- Is there anything the staff can think of that I might want to prepare for at home?
- Where and how can I get training for car seats, CPR, feeding pumps, oxygen, and other equipment?
- Do I know who is on my child’s care team and do I have their information?
- Do I know who to call (hospital, pediatrician, insurance, DME providers, friends family, etc.) when I need help?
- Do I have a support system for me at home?
- What are the warning signs to be aware of at home?
- Is insurance set up to continue when I’m at home?
- Do I have all the important papers I may need for my child’s medical care and insurance?
- Do I have a plan for follow-up visits?
For tips on life after discharge, read our companion article: Supporting Medically Complex Kids at Home.
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor


