Autism and Co-Occurring Diagnoses
It’s very common for children diagnosed with autism to experience other medical or mental health challenges and conditions. Data shows that having a co-occurring condition is much more prevalent in children with autism than in the general population, so it’s important to recognize these conditions, as they could stimulate or exacerbate symptoms and may also complicate interventions. To get some insight into co-occurring conditions, we sat down with Dr. Hitha Amin, neurodevelopmental neurologist at Children’s Hospital of Orange County (CHOC) Thompson Autism Center, and Dr. Emily Haranin, child and adolescent psychologist at Children’s Hospital Los Angeles and clinical assistant professor of pediatrics at Keck School of Medicine at USC.
Note to our readers: A recent article on the use of language in autism research documents a preference among some people with autism for language that refers to autism as a condition rather than a disorder — and, therefore, to refer to other conditions using the term “co-occurring” instead of “co-morbidity.” As Dr. Amin notes, autism is an umbrella term that describes individuals in many different circumstances; to adopt the most inclusive language, we use the term ”co-occurring.”
What are some common co-occurring conditions with autism?
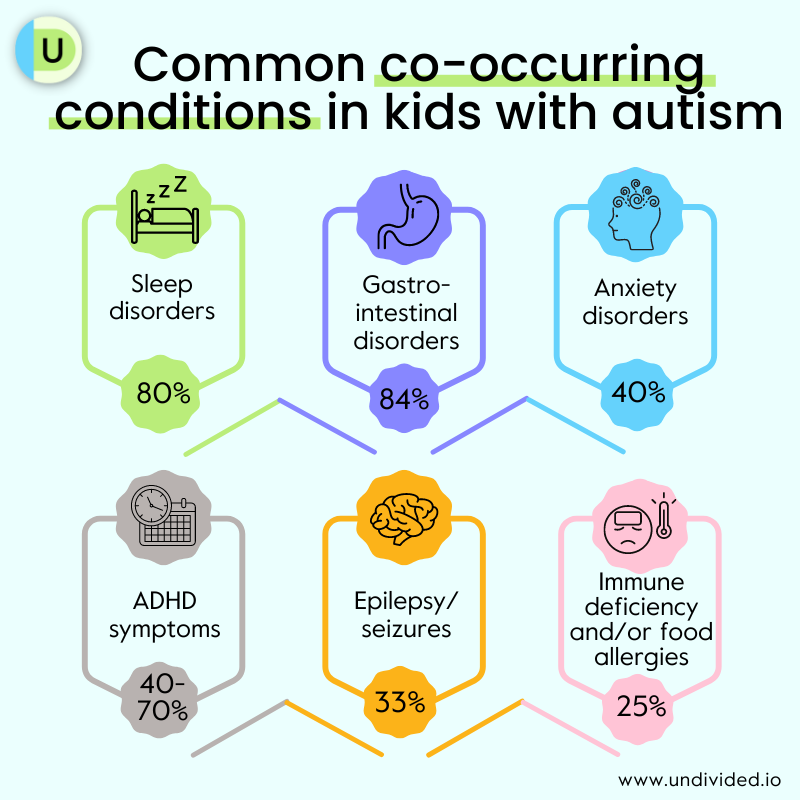
Research from the CDC tells us that more than 95% of children with autism have at least one co-occurring condition, with more than half having four or more conditions. While this will manifest differently in every child, co-occurring conditions can exacerbate the symptoms of autism and even delay the timing of diagnosis.
Because autism is diagnosed based on a scoring of symptoms, co-occurring conditions can also present as symptoms of autism. Dr. Amin explains that because of this, co-occurring conditions can augment a child’s symptoms. She explains, “Even if someone's been scored based on their symptoms, you may see a higher scoring on the autism symptoms just from having those co-occurring conditions. A lot of these co-occurring conditions can also be interrelated.”
An example of this is if a child with autism also has a sleep problem and a GI issue such as constipation, Dr. Amin says, “having that discomfort is going to worsen their sleep problems, and when their sleep is disrupted, they have more anxiety symptoms. What you may see is they don't really want to socialize at that point. So if they already had difficulties with social interaction, now it may worsen.” Being aware of and addressing related conditions can help families and medical professionals clarify the core symptoms of autism that are present, and thus determine the appropriate treatment plans and interventions.
The most common co-occurring conditions that present with autism include ADHD, anxiety, depressive disorders, epilepsy, sleep disorders, sight or hearing impairment or loss, and GI syndromes. Understanding how co-occurring conditions interact with autism is important in better understanding the experiences and symptoms a child is having. As Dr. Haranin says, “We want to treat the whole child and not just the diagnosis.”
For example, if a child is headbanging, it could be due to chronic, painful headaches (autistic individuals are 2.2 times more likely to have severe headaches) and the inability to communicate their symptoms. Similarly, food refusal or food selectivity could actually be the child reacting to a food allergy or intolerance.
Autistic individuals are also four times more likely to experience depression compared to the general population, affecting 7.7% of children and 40.2% of adults.
Do co-occurring conditions present differently in girls with autism?
Autism and ADHD
Both ADHD and autism are neurodevelopmental conditions that present in childhood. Studies show that ADHD is one of the most common co-occurring conditions of autism, with 40-70% of autistic people having significant ADHD symptoms. The coexistence of ADHD and autism can also complicate diagnosis, since ADHD traits may mask those of autism.
Dr. Haranin tells us that when approaching ADHD treatment, it’s important to first make sure the child is ”receiving high-quality intervention to support any challenges that are associated with that autism diagnosis,” and then seeing which co-occurring condition is causing the biggest concern, specifically when it comes to behavior, and making sure there is treatment and support in place for it.
Treatment may include medication (for ADHD), but psychological and environmental interventions are also highly recommended, such as psychoeducation, behavioral parent training and support, behavioral and environmental interventions specific to the child’s needs, and therapy. Treatment may also combine medication and behavioral therapy, but the aim is to make sure the treatment is as effective as possible.
Dr. Amin explains that if a child’s attention span makes behavioral therapy less effective for them, and a clinician finds that medication to treat ADHD symptoms is appropriate, “then we may use that approach where we try to combine treatment modalities, like a behavioral and medication approach to best address the symptoms. Again, this would always be tailored to a particular child and their family. So it may be hard to generalize, but we do see that children with ADHD and autism as a co-occurring condition may be more likely to be on medication.”
She adds that it can be extremely helpful for a child who has co-occurring autism and ADHD to work with a healthcare professional who has experience treating both conditions. “As we manage these co-occurring conditions better, we may see a better involvement in therapies as well,” Dr. Amin says.
To learn more about ADHD, read our article ADHD 101.
Autism and anxiety
Anxiety disorders affect an estimated 40% of autistic children and teens, with some studies showing percentages as high as 84%, compared to about 25% of typical children. According to one study, anxiety in children with autism might present as “sleep problems, self-injurious behavior and parental stress, insistence on sameness, and sensory under-and over-responsiveness.” The most common co-occurring anxiety disorders are social phobia, specific phobias, generalized anxiety disorder, separation anxiety, and obsessive-compulsive disorder (OCD).
While anxiety may appear prominently in autism, it isn’t part of the diagnostic criteria. Symptoms of autism can masquerade as anxiety, or vice versa, making evaluation and diagnosis more complex. For example, social anxiety (avoidance of social situations or social judgment) may be mistaken as a social communication deficit in autism, or repetitive behaviors within autism may overlap with compulsions in OCD. According to a report in Spectrum, “Children with autism may be inherently more likely to develop anxiety than their typical peers. But the overlap in features between the two conditions makes diagnosing anxiety extremely difficult.”
Newer research measuring anxiety specific to autistic children found symptoms of anxiety that don’t fit the standard diagnosis. This prompted psychologist Connor Kerns and her colleagues to create an adapted and expanded version of the Anxiety Disorders Interview Schedule (ADIS) to flag those atypical anxiety traits: fear around routine, novelty, and restricted interests; fear of social situations without concern for social rejection; unusual specific fears; and compulsive behaviors with no clear function.
Why is this important? Knowing the difference between traditional and more unique anxiety symptoms in your child may help you better notice when anxiety is present, even if it doesn’t look like what you might expect anxiety to look like. It may also help you navigate the process of diagnosing co-occurring anxiety and cater treatment interventions to better fit your child’s needs.
Autistic children may have difficulty understanding, managing, and/or communicating their emotions, so identifying anxiety triggers and symptoms is the first step. The most common treatment for anxiety in children with autism is cognitive behavioral therapy (CBT), with modifications for each unique child as well as parental involvement and social skills training. Other recommended interventions can include relaxation techniques, visual tools and Social Stories, and safe exposure to feared triggers.
How should parents manage autism as a secondary diagnosis?
If your child has a primary diagnosis such as Down syndrome, Fragile X, cerebral palsy, bipolar disorder, or drug-resistant epilepsy, they may receive a secondary diagnosis of autism. Dr. Amin advises that with each of these conditions, it's important to deal with the underlying conditions.
For instance, she explains, it’s important with Down syndrome to first consider medical treatment for other common co-occurring conditions, such as hypothyroidism. Once these issues are addressed, if a diagnosis of autism is still appropriate, making that diagnosis can allow for the appropriate behavioral therapy to be provided, which can address areas of need such as social skills.
Can co-occurring conditions be a misdiagnosis?
Dr. Amin tells us that there is always a possibility of misdiagnosis, and this is particularly true when a child has co-occurring conditions. For example, she says, “if we think of how one of us might behave in a setting that causes a lot of anxiety, we may do things like not make eye contact. We may appear a little more withdrawn. So we do see that children may appear to have features that suggest autism.” Some symptoms of autism that can be commonly misattributed to other conditions include:
- Difficulty with social interactions (diagnosed as social anxiety disorder)
- Difficulty with verbal/non-verbal self-expression (diagnosed as a learning disability)
- Picky eating (diagnosed as an eating disorder)
- Poor social skills (diagnosed as ADHD)
- Challenges with relating to others (diagnosed as a personality disorder)
- Repetitive behaviors (diagnosed as obsessive compulsive behavior)
- Difficulty managing emotions (diagnosed as a mood disorder)
- Sensory sensitivities (diagnosed as sensory processing disorder)
- Trouble picking up on social cues (diagnosed as schizophrenia)
For this reason, it is important to have a comprehensive evaluation that takes place over several sessions.
How to approach autism diagnosis and treatment
It may not be easy to identify co-occurring conditions in children with autism due to problems in communication, ambiguity of symptoms, or changes over time. Many symptoms present in cycles or at different developmental stages, but early identification and treatment can help a child learn the foundational skills they need to grow. Early intervention also gives providers the opportunity to offer the most appropriate evidence-based treatment.
“Since [autism] presents with multiple behavioral characteristics, professionals often miss the big picture of autism and, instead, diagnose small pieces of the picture separately — for example, obsessive compulsive disorder (OCD), social anxiety, eating disorder, bipolar disorder, or attention deficit hyperactivity disorder (ADHD or ADD),” writes Theresa Regan, Ph.D. in ADDitude Magazine.
A pediatrician may recommend that you see a specialist who is qualified to evaluate and diagnose autism and its co-occurring conditions. One option is autism-specific centers or clinics, which, as Dr. Amin tells us, allow for a longer period of evaluation: “The goal of having a center that does these evaluations is because we have the ability to have a period for evaluation. Sometimes in a community pediatrician’s office, they may not have the bandwidth to be able to do a one-hour or two-hour evaluation for the child.”
Autism centers such as CHOC Thompson Autism Center or the Boone Fetter Clinic at CHLA can provide families with a team approach to autism care. Dr. Amin emphasizes that it is a family preference and does depend on where you live, noting that it may be difficult for families to travel to a center that does everything under one roof.
When it comes to treatment, Dr. Haranin recommends focusing on the biggest concerns: “Whenever we’re approaching treatment for coexisting conditions, we want to see which condition is causing the biggest concerns at the time. What are those specific behavioral concerns? Let’s make sure treatment is in place for that, and a child is receiving support for that.”
She also highlights the importance of creating a partnership between the family and a child’s providers. “This is another reason why it’s really valuable to have a team involved,” she says. “Talking about any language delays or alternative communication or other aspects — it’s important that we take all of that into consideration and not treat children like they're in little boxes. We want to treat the whole child and not just the diagnosis. And so when we’re talking about treatment, it really has to be more fluid.”
To learn more, check out our article Diagnosing Autism as well as Autism 101 and Getting a Child with Autism the School Supports They Need.
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor