IEP Related Services: The Difference Between School-Based and Clinic-Based Services
When determining which services our child needs, we often find ourselves wondering about the differences between school-provided and private therapies. What can we expect of each one — and should we pursue both? We spoke with Amanda Prine, OTR/L; Melissa Epstein, OTR/L-MA; Anne Osborn, DPT; and Kimberly Gardener, OTD, SWC, CAS — all of whom have experience in both settings — to better understand their benefits and limits.
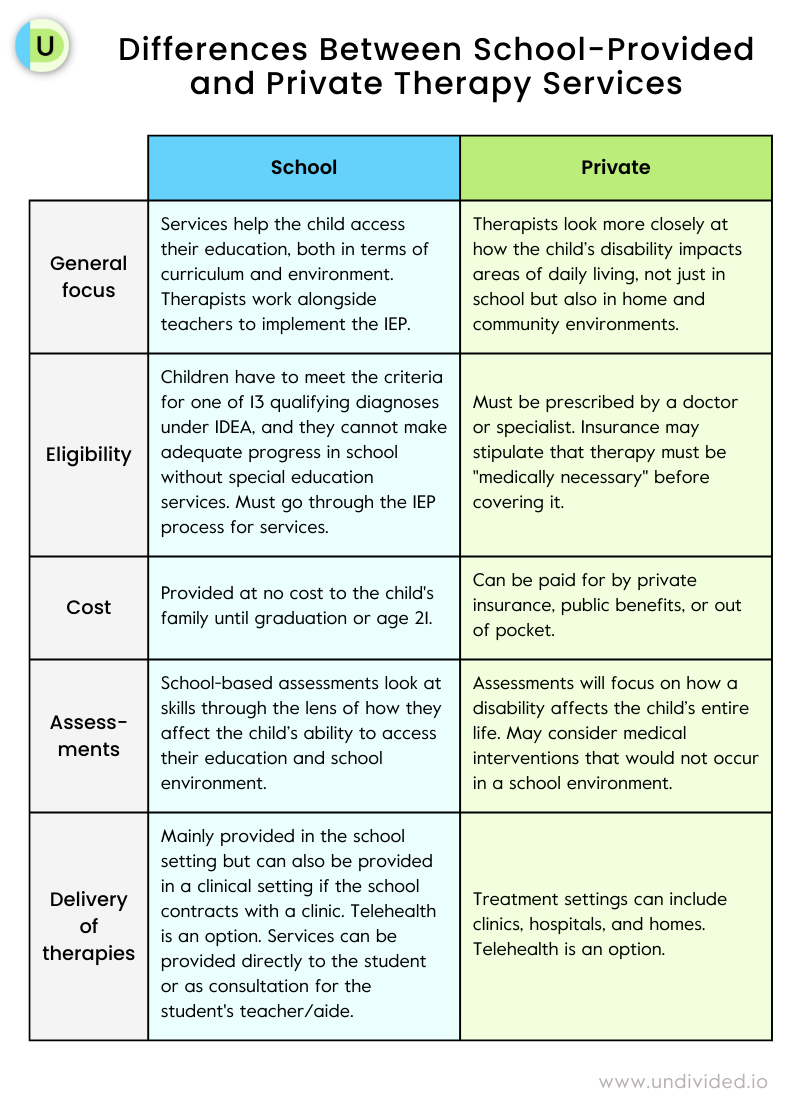
General focus of services and therapies
School
The focus of school-provided services is on the child’s ability to access their education, both in terms of curriculum and environment. Can they physically access the classroom, playground, and bathroom safely? Can they hold a pencil, write, stay seated in their chair, and participate in lessons? Every skill they will need to succeed is evaluated and treated through the lens of education.
Therapists work as part of the child’s care team alongside the teacher and other service providers on developing and implementing the child’s IEP. Documentation is related to the child’s IEP rather than insurance requirements, and uses educational terminology.
Private therapy clinic
Private Therapy Clinics look more closely at how the child’s disability impacts areas of daily living — such as feeding, dressing, sound production, sensory processing, general strengthening, fine and gross motor skills, and balance and coordination. Clinical services look at “not just the child’s role as a student, but their role in home and community environments,” explains Amanda Prine, OTR/L, an occupational therapist who currently works for a school district but has worked in private clinics.
Clinical therapists are the direct provider. Documentation is often dictated by setting and insurance guidelines/requirements, and uses more medical terminology.
Eligibility and cost of therapies
School
To receive school-provided services, children have to meet the criteria for one of 13 qualifying diagnoses under IDEA, and cannot make adequate progress in school without special education services. You must go through the IEP process to receive services, even if the school district is paying for outside therapy.
Children have to qualify for services through a school-based need, explains Melissa Epstein, OTR/L-MA, owner of Thrive! Occupational Therapy. “If your child holds their pencil incorrectly but can keep up with the class and their writing is legible, they won’t qualify for OT. But if it’s inhibiting them from being able to write, they might qualify.”
School-provided services are available up to high school graduation or the age of 21, and are provided at no cost to the child’s family.
When communicating the necessity for school-based PT to be included in your child’s IEP, consider what they need to access their education and the school environment.
- Can your child sit in their chair in the classroom?
- Are they able to safely move around the school?
- Can they successfully access necessary learning materials?
- Are they safe on the playground or schoolyard?
“The school is only concerned with the school’s goals,” adds Leslie Lobel, Director of Health Plan Advocacy at Undivided. “If you want PT to take place in school, your child’s IEP goals will have to be framed in a way that will be acceptable to the IEP team.”
Private therapy clinic
Private, clinic-based services are prescribed by a physician.
Services are available for all ages, and are funded in many ways: schools (if the school does not have services on site), private insurance (either in-network or out-of-network, where superbills can be submitted for partial reimbursement), or government services.
If a clinic accepts insurance, they might be bound by what the insurance provider thinks is medically necessary, says Kimberly Gardener, OTD, SWC, CAS, who worked with LAUSD before opening her own clinic, OT 4 Kids. Gardener advises parents to use private insurance if they have it: “Sometimes you can access clinic services through Medicaid benefits, but a lot of facilities don’t accept it.” If a child is age three or under, a family can see if their child qualifies for state early intervention programs.
Assessments
School-based assessments look at skills through the lens of how they affect the child’s ability to access their education and school environment, Epstein says. “If a child is recommended for an assessment for school-based therapy due to difficulty remaining in a chair and inability to hold a pencil, the therapist would give a standardized test that provides scores on their current overall level of fine/gross motor skills and sensory processing skills. Specifically, they look for deficits that negatively impact their ability to fully access and participate in their education.”
Private, clinic-based assessments might use the same test but will focus on how it affects the child’s entire life: “The clinic will look at how it affects their ability to sit at a table and participate in a family meal, whereas the school looks at whether they’re able to eat their lunch,” Epstein says. A clinical assessment looking at medical interventions would not occur in a school environment, adds Prine.
Delivery of therapies
School
The majority of school-provided therapy services are provided in the school setting but can also be provided in a clinical setting if the school contracts with a clinic. These services can also be provided through telehealth. “We've created fun games and activities to do at home that address various impairment areas, including strength, balance, coordination, and range of motion to help prevent regression in their gross motor skills,” says Anne Osborn, DPT, a physical therapist who works with school-based and private clients through TherapyWest.
Services can be provided directly to the child or on a consultative basis, where the therapist provides suggestions to the teacher and classroom aides. “School-based therapy can look very different,” Prine says. “It can be more restrictive, where kids are pulled out of class and worked with one-on-one or in small groups, or a push-in model where the therapist gives instruction to the aides in the classroom.”
Private therapy clinic
Treatment settings typically include clinics, hospitals, and homes. Telehealth is another option for many families. Some clinics also provide in-home services or the option to meet in a yard or park.
Some kids’ presentation does not work well with telehealth, Epstein says. “If you have a kiddo with autism and attentional issues, it can sometimes be very hard to help them virtually. Telehealth works best when the parent or caregiver is an active participant. The therapist is leading the session but describing to the parent how to do the physical cues.”
What each therapy can provide
Occupational therapy
In schools, Prine says she looks at what kinds of supports are already in place in classroom environments and curriculum — does the child need an accommodation, like extra time to get between classrooms or more time to complete assignment?
Private, clinic-based occupational therapists look at sensory issues and the child’s “occupation” during play and as a family member, including skills such as riding a bike or playing sports. “Feeding skills, such as expanding types of foods the child will eat, would be worked on in a clinic, but not at school — even though nutrition is part of school, it’s not helping you access the curriculum,” Prine adds.
Physical therapy
A school-based physical therapist looks at how the child physically accesses their school environment, explains Osborn. Can they safely navigate the classroom and school grounds (curbs, ramps, stairs, etc.), physically access educational materials, negotiate busy hallways and common areas, and safely access playground equipment, cafeterias, and restrooms? Osborn says they also assist with environmental adaptations, ordering and monitoring equipment (such as adaptive seating devices, gait trainers, and modified tricycles), and training staff on the use of any assistive equipment, handling, and transfers (for example, transferring from the wheelchair to the toilet and back).
Clinic-based PT looks at medical considerations of the child’s disability, such as stretching to help prevent crouch gait in cerebral palsy; strengthening to help a child sit, stand, and walk as independently as possible; working on balance; troubleshooting equipment needs; and working to safely navigate different home and community environments.
Speech therapy
A school-based speech therapist focuses on social pragmatics, reading skills, and receptive language — meaning how they process the language they’re hearing and how they follow directions, Gardener says. Speech and language services are often conducted in a group with similar-age peers.
Clinic-based speech therapists have more freedom to treat children using a variety of therapeutic modalities such as PROMPT, in which the therapist uses manual cues on a child’s lips, jaw, tongue, throat, and cheeks to help guide difficult sound productions. They might also have access to swings and other equipment to motivate speech through movement.
Clinic-based speech and language services are often one-on-one, allowing clinicians the ability to individualize sessions. Nikki Rubin, a speech and language pathologist at Speech 4 Kids, says they incorporate preferred activities, games, and toys into the session to increase participation and motivation.
Advice to parents of kids with IEPs
Make sure that school- and private, clinic-based therapists are communicating with each other. Gardener says that a lot of families don’t know that schools and clinics can and should collaborate as much as possible. Prine agrees: “School therapists should talk to clinics and share information, such as any outside reports the family had done. Most therapists I know are happy to have the opportunity to talk to outside therapists to gain more information.” Epstein says she often talks to school therapists on the phone, even if it’s just a call every few months to check in. She also says to make sure the clinic-based therapist has a current copy of your child’s IEP. “Constant communication with the IEP team, therapists, and the family is huge,” Osborn says. “When problems arise with IEPs, it’s often because there isn’t communication between the family and the therapist." Lobel adds, “If you’re having PT both privately and PT based on IEP goals, you want to make sure that you facilitate communication between those two providers so they’re not working at cross purposes with your child.” The two should always be reporting progress updates to each other.
Be proactive if you feel your child needs services, Epstein says: “Everyone is entitled to an IEP evaluation.” Gardener agrees: “A lot of parents are nervous about diagnosis and stigma, but early intervention is the best.”
Be open to both types of services: “A lot of parents say their child doesn’t need clinic-based services because they get services at school or vice-versa, but I encourage parents to access as many options as possible because it’s going to help,” Epstein says. “We work on similar things in a completely different way.”
Check with your pediatrician or insurance to find providers in your network so you can get services that aren’t covered by the school, Prine says. State agencies, such as Regional Center in California, are typically a payer of last resort, which requires a denial letter from your insurance.
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor