Big Changes to Fee-for-Service Medi-Cal: Update!
If your child is a Medi-Cal recipient with private health care coverage, you have likely been notified by now that you must assign your child’s Medi-Cal to a managed care plan instead of fee-for-service or “straight” Medi-Cal coverage.
This is a big change. For over a decade, Medi-Cal recipients with other health coverage have been exempt from mandatory enrollment in a managed care plan. On January 1, 2022, a program called CalAIM went into effect to streamline the delivery of Medi-Cal services in the community, including a requirement that most recipients enroll in a plan even if they were exempt previously. For those with other health coverage who are enrolled via Medi-Cal Home and Community-Based Services (HCBS) waiver — including the institutional deeming waiver — and for those who are dually eligible for Medi-Cal and Medicare, this change took effect January 1, 2023. Going forward, only a small number of recipients will remain under fee-for-service Medi-Cal.
Here’s what families need to do now to prepare for the changes.
How to choose a Medi-Cal managed care plan
Your child should have received a packet from Medi-Cal Health Care Options advising you of your county’s Medi-Cal managed care plan options. In the past, families of children with other health coverage have been advised to disregard this packet and decline to select a plan. This time, you will need to proceed with the plan enrollment process.
NOTE: Many parents have reported that their packet still includes language from previous years stating that “You or a member of your family cannot choose a health plan if you are a member of a commercial health plan through private insurance.” This is an error! If you have received this packet, you must choose a plan.
If you currently use fee-for-service Medi-Cal as secondary coverage for any of your child’s providers, you should already be asking providers whether they intend to participate in a Medi-Cal managed care plan. Don’t forget to check not just with your child’s treating physicians but also with service providers for OT, PT, speech therapy, ABA, home health (e.g., private duty nursing), and any other health care services you utilize on a regular basis. Knowing which providers will accept both your primary health insurance and a Medi-Cal plan can help you choose the most appropriate plan for your child.
Hear tips for going about the process in this clip from Public Benefits Specialist Lisa Concoff Kronbeck:
As you make your decision, it’s worth noting that several of Medi-Cal’s current managed care insurers, including Health Net and Blue Shield of California, may not see their Medi-Cal contracts renewed in some counties due to new, stricter provisions intended to improve transparency and patient care. Here is a table with each county’s current plans and what they are estimated to be by 2024. You may wish to take these changes into consideration to avoid facing another potential upheaval in the next couple of years.
It’s important to know that if you fail to select a plan by the due date, the county will automatically choose a plan for you.
NOTE: Some additional changes will roll out in 2024, mostly changes to county plan options in several counties. Per DHCS’s email to stakeholders on September 1, 2023, about 243,000 members will receive packets to choose a new plan in their county, about 420,000 will be assigned automatically based on their county plan, and about 500,000 Los Angeles County residents will be transitioned from HealthNet to Molina as new contracts go into effect.
To make your selection, or to choose a different plan if you were automatically enrolled, you can call Medi-Cal Health Care Options at (800) 430-4263.
How to request a Continuity of Care agreement
Children who are in active treatment for a medical condition can request Continuity of Care for up to 12 months if their fee-for-service Medi-Cal provider is not contracted with any county plan but is willing to enter into a single case agreement with the selected managed care plan, and they can agree on a rate. Note that a Continuity of Care agreement cannot be requested until after the managed care plan is active. We have been advised that if a child is not in active care (for example, in remission or being monitored long-term), they will be transitioned to a provider of the same specialty within the managed care plan. If the managed care plan does not have the appropriate specialist, they need to contract with one; you can request that they enter into an ongoing single-case agreement with your child’s current provider.
The DHCS Continuity of Care FAQ lays out what must happen for a successful Continuity of Care request:
- The managed care plan is able to determine that the child has an ongoing relationship with the provider. “Ongoing relationship” means the child has seen the provider at least once in the previous 12 months before enrolling in the managed care plan.
- The provider is willing to accept the managed care plan’s contract rates or Medi-Cal fee-for-service rates, whichever is higher.
- The provider meets the managed care plan’s applicable professional standards and has no disqualifying quality-of-care issues.
NOTE: The Continuity of Care request process is specifically for prior fee-for-service Medi-Cal providers, not all out-of-network providers. You will not be able to use this process to get a Medi-Cal managed care plan to cover out-of-pocket expenses billed by a provider who did not accept fee-for-service Medi-Cal before the transition.
Potential roadblocks when switching to a Medi-Cal managed care plan
Below are some issues that may arise during and after the transition and how to approach them proactively:
Currently, Regional Centers provide ABA services for children enrolled in fee-for-service Medi-Cal if their primary insurance will not cover ABA. Most often, the private insurance has denied services because the child does not have an autism diagnosis. ABA providers generally don’t contract directly with fee-for-service Medi-Cal; instead, Regional Center is the designated Medi-Cal ABA provider for children with FFS Medi-Cal. However, children in a Medi-Cal managed care plan are covered for medically-necessary ABA services regardless of diagnosis. Once your child is enrolled in a plan, you will need to use a provider who is contracted with that plan. Now is the time to ask your provider if they intend to contract with a Medi-Cal managed care plan, and if so, which one.
- TIP: You can request a Continuity of Care agreement if your ABA agency doesn’t participate in a managed care plan and switching to the managed care plan’s contracted ABA agency would result in a significant lapse in care — for example, if the new company has a long wait list. We have been told by at least one Regional Center that continued Regional Center coverage for ABA may be approved temporarily on a case by case basis while families complete the process of either switching their child to a plan-contracted agency or requesting Continuity of Care coverage from the plan.
Children receiving home nursing services will have a reassessment by the managed care plan to ensure that they are receiving the right number of hours. It is the managed care plan’s responsibility to make sure the hours are staffed. With the national LVN shortage, this is a great example of a situation where a Continuity of Care agreement can help prevent disruption in care. While a Continuity of Care agreement cannot be requested until after the managed care plan is active, it can still be helpful to do your homework and find out whether the nursing agency will participate in a plan or would be willing to enter into a Continuity of Care agreement.
Durable medical equipment (DME) should be purchased from a supplier who accepts both the private insurance and the managed care plan. After the private primary plan pays its part, the managed care plan should pay the out-of-pocket portion up to the Medi-Cal rate, even if the prescription came from a provider outside of the managed care plan. As with other Medi-Cal services, you should not be billed for any unpaid balance after the primary insurance and the managed care plan have paid their portion. You should work with your plan’s enhanced care management coordinator if you have concerns about funding DME.
A lot of families have asked whether they will be able to continue to see their child’s specialists once they enroll in a managed care plan. Because Medi-Cal is acting as secondary insurance, Health Care Options reports that children should not require a referral from an in-network primary care doctor to see a specialist as long as the specialist accepts both the primary insurance and the Medi-Cal plan.
NOTE: Everybody’s due date seems to be a little different depending on when their packets went out, so you should check your own packet to confirm when you need to choose a plan.
You should also know that even after your child transitions to managed care, they will access pharmacy benefits and incontinence supplies via Medi-Cal RX, the same pharmacy network that serves fee-for-service recipients. This is a statewide policy change that affects all Medi-Cal recipients and gives patients access to a more expansive network of pharmacies.
We hope this clarifies the upcoming changes to Medi-Cal enrollment. We realize you may still have questions about how coverage and coordination of benefits will work for children who have a private PPO as their primary insurance and Medi-Cal managed care as their secondary coverage. We have the same questions! As always, we are working hard to get more information and bring it back to you.
Takeaways
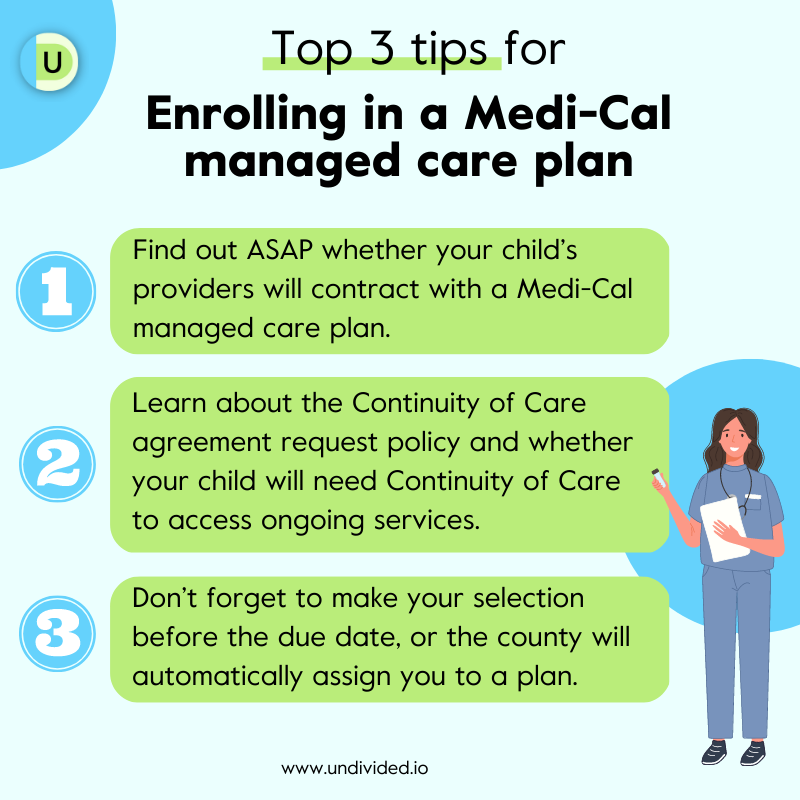
- Find out ASAP whether your child’s providers will contract with a Medi-Cal managed care plan.
- Familiarize yourself with Continuity of Care policies and criteria. Continuity of Care requests may be critical in ensuring that your child has access to ongoing treatment and services during this transition.
- Don’t forget to make your selection before the due date, or the county will automatically assign you to a plan and it may not be the one you prefer. You can always switch to a different plan, but it’s easier to be proactive than to fix an unexpected enrollment. Remember that everybody’s due date seems to be a little different depending on when their packets went out, so you should check your own packet to confirm when you need to choose a plan! Once you make your selection, the plan should be active by the following month. So if you haven’t made a decision yet, you may want to wait until after January 1 if your due date permits.
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor