Medi-Cal Terms & Services Glossary
Medi-Cal, California’s Medicaid program, provides millions of Californians with low-cost and free healthcare services based on individual factors including income, disability, and adoption and/or foster care status. Medi-Cal is funded equally by the state and the federal government, and can be used as primary or secondary insurance, depending on your existing insurance and your child’s health needs. Medi-Cal will always be secondary to any other health care coverage.
As secondary insurance, Medi-Cal can bridge gaps in primary coverage by eliminating co-pays and other out-of-pocket expenses for medical visits and supplies when your child visits Medi-Cal-contracted providers. (To learn more about this, check out our article How to Use Medi-Cal as Secondary Insurance.) Medi-Cal also offers programs such as In-Home Supportive Services (IHSS), which provides people with disabilities with home-based care, paramedical services, and more.
We know that navigating the healthcare system can be both time-consuming and frustrating, especially when your child relies on insurance to access the medical services they need to lead healthy, happy lives. Here, we hope to take some of the work from your plate so that you can more quickly find and access the Medi-Cal services and supplies your child needs — and, importantly, learn how to appeal if Medi-Cal denies that coverage.
Medi-Cal terms to know
Aid paid pending appeal — If you receive a notice of action (NOA) reducing or terminating a benefit or service that you are already receiving (including Medi-Cal eligibility), in most cases you can continue to receive the benefit during the appeal process if you appeal within ten calendar days of receiving the NOA. You should submit the appeal request in writing so that there is proof it was completed, and you may also wish to make a note on the appeal form that you are requesting aid paid pending appeal.
Coordination of benefits (COB) — This is the method that insurance plans use to provide coverage and determine payment responsibilities for someone who is covered by more than one health plan. To ensure that insurance companies and other third parties pay their share, the state collects information on any pre-existing coverage whenever someone applies for medical assistance. If a family applies for Medi-Cal for their child, they must also show proof of any insurance or other third-party coverage.
Fair hearing / state hearing — If you disagree with a Notice of Action or with the way your Medi-Cal benefits and/or services are being handled, or how services have been denied or modified, you can request a fair hearing, also referred to as a “state hearing.” The request must be filed within 90 days of receiving the Notice of Action. You may be able to file after 90 days if you have a good reason, like illness or disability. You can also complete the "Request for State Hearing" on the back of the NOA. For more information on how to request a fair hearing, see our article on Medi-Cal appeals as well as the DHCS website.
- If your child is enrolled in a Medi-Cal managed care plan, you must exhaust your appeal rights with the managed care plan before filing for a state hearing. For more information about appealing managed care decisions, see All County Letter 21-011.
Full-scope Medi-Cal — Full-scope Medi-Cal includes the full range of services offered under the program, as opposed to some Medi-Cal programs that are limited only to specific types of care. Full-scope Medi-Cal provides free or low-cost health coverage including medical, dental, mental health, and vision care. It also covers alcohol and drug use treatment, drugs that your doctor orders, and more. Children in foster care and former foster youth up to age 26, pregnant women, people who are blind or have disabilities, people 65 and over, and people who get CalWORKs (AFDC) or Supplemental Security Income (SSI) are eligible for full-scope Medi-Cal. Learn more at www.dhcs.ca.gov.
Institutional deeming waiver — When a person with disabilities applies for income-based Medi-Cal, the state will “deem” parental or spousal income and resources to the individual when determining their eligibility. This means that even if the person doesn’t have their own income and resources, they may still be ineligible if their household income as a whole is too high. When a person with disabilities lives in an institution such as a hospital or nursing facility, only their own income and resources can be counted. “Institutional deeming” means that when a person with disabilities qualifies for placement in a state institution, the state will assess their eligibility as if they were already there. This approach allows more people with disabilities to receive services and supports at home and in the community, thus avoiding unnecessary institutionalization. Medi-Cal’s Home and Community-Based Services for the Developmentally Disabled Waiver (HCBS-DD) is one of several waivers that use “institutional deeming” criteria to provide greater access to Medi-Cal for people with disabilities regardless of family income, as long as the individual’s personal income and resource levels fall below program thresholds.
Managed care — Managed care is a program in which all care exists within a limited network of providers and clinics that participate in that specific plan. You may be familiar with this type of program already; outside of Medi-Cal, it is usually referred to as a “Health Maintenance Organization” or “HMO.” Medi-Cal managed care provides accessible and cost-effective health care through streamlined delivery systems by contracting for health care services through established networks of organized systems of care, which emphasize primary and preventive care. You will receive an enrollment packet, a Benefits Identification Card (BIC), and a managed care health plan card along with instructions for finding in-network providers. New Medi-Cal recipients are encouraged to call Health Care Options and select a plan. If they fail to do so, one will be chosen for them.
Notice of Action (NOA) — An NOA is a written notice providing an explanation of eligibility, coverage, or benefits to Medi-Cal applicants and beneficiaries. An NOA includes the decision and effective date of coverage as well as any changes made in eligibility status or level of benefits. If the NOA is denying or terminating a benefit, it should provide a reason for the denial or termination. It also includes information about hearing rights and how to appeal the decision if you disagree with the determination. See a walkthrough of an example NOA here.
- If you don’t understand your NOA or have questions about your eligibility, you can contact your local county office at the phone number listed on the NOA. You may also find contact information on your Local County Office website.
Prior Authorization (PA) — Prior authorization is a request for coverage of Medi-Cal Rx pharmacy benefits or services. This includes documentation stating that the requested pharmacy benefit or service is medically necessary for the Medi-Cal beneficiary.
Share of Cost (SOC) — People with disabilities whose countable income (the income Medi-Cal is allowed to look at for eligibility) is too high to qualify for a free Medi-Cal program may be eligible to enroll with a Share of Cost (SOC). A Share of Cost is the amount of money an individual is responsible to pay toward their medical related services, supplies, or equipment every month before Medi-Cal begins to pay. For more information about SOC, see this flier. Be aware that the monthly Share of Cost is often prohibitively high unless the individual has extensive medical costs each month.
Straight or fee-for-service Medi-Cal — Until January 1, 2023, recipients who had private health insurance as their primary plan could opt out of managed care and enroll instead in fee-for-service Medi-Cal (sometimes referred to as “straight Medi-Cal”). Medi-Cal will always be secondary coverage for children with private primary insurance, but it can help fill some of the funding gaps by eliminating copays and many other out-of-pocket expenses when your child sees Medi-Cal-contracted providers. If a child has multiple insurance plans, Medi-Cal is always the last provider to be billed. As of January 1, 2023, most Medi-Cal recipients are required to enroll in a managed care plan unless they have a Share of Cost or receive Medi-Cal through the state’s programs for foster and former foster youth.
Treatment Authorization Request (TAR) — Some services and medications require prior authorization by Medi-Cal. Authorization requests are made with a Treatment Authorization Request (TAR). These are based on federal and state law. There are two ways to submit a TAR for review: electronically or by paper. The provider will submit the TAR and check its status. If the TAR is denied and you disagree with the decision, you may be able to request a fair hearing. If you have the TAR number, you can check on the status of your request.
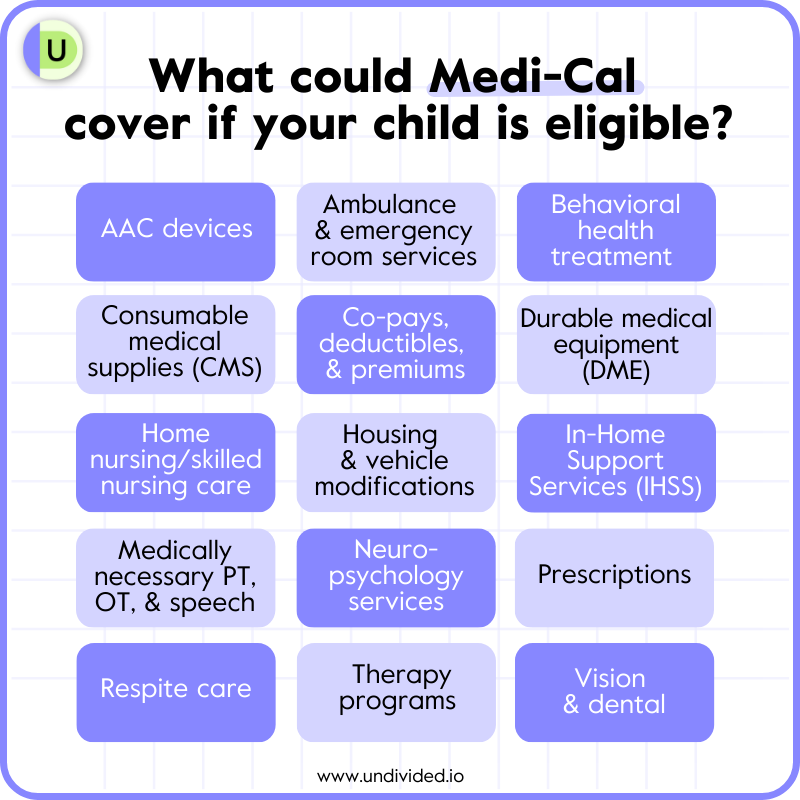
Services covered by Medi-Cal
AAC devices
Augmentative and alternative communication (AAC) devices help children whose disabilities prevent them from using oral speech to communicate with others. Some common non-electronic and electronic AAC devices include symbol boards, choice cards, alphabet charts, AAC apps on mobile devices, and speech-generating communication devices. Some AAC devices produce speech based on text a person types while others produce speech based on symbols a person selects.
Medi-Cal considers AAC devices to be durable medical equipment. As long as your child’s physician determines that an AAC device is medically necessary, Medi-Cal should cover it, although they may request additional documentation and/or further assessment. Because of their cost, all AAC devices require prior authorization from Medi-Cal. As always, Medi-Cal will require that your child’s primary insurance be billed first.
If Medi-Cal doesn’t approve a prior authorization for an AAC device, you can request a hearing to appeal the decision.
Ambulance and emergency room services
Medi-Cal can cover emergency medical transportation in cases when someone cannot use typical public/private transportation methods to access urgent medical care.
Medi-Cal specifically covers emergency ground transportation, or ambulance rides, to the nearest hospital or acute-care facility capable of meeting a recipient’s medical needs, even if it doesn’t contract with Medi-Cal. In cases where a facility doesn’t contract with Medi-Cal, a patient will be transferred to a Medi-Cal-contracted hospital/acute-care facility as soon as they become stable for transport.
Before making a coverage determination, Medi-Cal will require you to submit an Emergency Statement. Make sure to include the following in your (typed-out) statement:
- The nature of the emergency
- The name of the hospital/acute care facility where your child received care (do not use an acronym for the hospital name)
- The name of the physician responsible for your child’s emergency care (this isn’t required for all emergency transportation claims)
If Medi-Cal doesn’t approve coverage for emergency transportation services, you can request a hearing to appeal the decision.
Medi-Cal may also cover some non-emergency transportation, such as if a child requires a wheelchair and the family doesn’t have an accessible vehicle. You can find more details on the DHCS Transportation Services page.
Behavioral health treatment (BHT)
Medi-Cal typically covers “all medically necessary behavioral health treatment (BHT) for eligible beneficiaries under 21 years of age” so long as the therapy is evidence-based, according to California’s Department of Health Services.
Like other services, behavioral health treatments including applied behavioral analysis (ABA) require prior authorization from Medi-Cal and must be deemed medically necessary by your child’s physician or psychologist to warrant coverage.
If Medi-Cal doesn’t approve a prior authorization for behavioral health treatment, you can request a hearing to appeal the decision.
Consumable medical supplies (CMS)
Consumable medical supplies (CMS) are any “non-durable” or single-use medical supplies. CMS must be prescribed by a physician to be considered for Medi-Cal coverage. Examples include syringes, needles, catheters, medical gloves, diabetic test strips, and wound dressings. Here is Medi-Cal’s list of covered products.
If the specific medical supplies your child needs are not listed, you can try asking your child’s physician to request prior authorization. If your request for prior authorization is denied, you can request a hearing with Medi-Cal to appeal the decision.
As with all services and supplies, Medi-Cal will not fund CMS unless your primary insurance has denied coverage. Be sure to include a written denial from your primary insurance when applying for Medi-Cal coverage. For more information, check out our article Using Medi-Cal as Secondary Insurance.
Co-pays, deductibles, and premiums
Many individuals receiving Medi-Cal coverage, especially kids with disabilities, pay no premiums, co-pays, or other out-of-pocket costs.
Whether your child qualifies for income-based (no cost) or low-cost Medi-Cal coverage depends on the nature of your child’s disability, the level of their support needs, and your household size and income. To go deeper into the nitty gritty of the Medi-Cal eligibility determination process, check out our Medi-Cal 101 guide.
Children with disabilities whose household income exceeds the Federal Poverty Level (FPL) average can still qualify for free full-scope coverage through an institutional deeming waiver, which only considers the child’s own personal income and resources, not the entire household’s. The majority of children with disabilities who qualify for waiver-based Medi-Cal will enroll via the waiver for individuals with developmental disabilities (HCBS-DD). You can read more about that waiver program in our article Medi-Cal’s Institutional Deeming Waiver 101.
- The HCBS-DD waiver is available to Regional Center clients ages 3 and up who have two or more qualifying conditions in the areas of self-help, motor functioning, social/emotional functioning, special health care conditions, or extensive medical needs. The waiver is also available to Regional Center clients under age 3 who have been diagnosed with a developmental disability that will continue to qualify them for Regional Center services past the age of 3 and who have significant medical/health care needs. Medically complex children who are not Regional Center–eligible may still qualify for institutional deeming under a different waiver for individuals who meet the criteria for placement in a skilled nursing facility.
If your household size and income exceed the Federal Poverty Level (FPL) average and your child’s disability and/or support needs do not meet waiver criteria, they will not qualify for free Medi-Cal coverage. They may, however, still qualify for coverage with a monthly Share of Cost (technically, this is called the Medically Needy Program, or ABD-MN). Share of Cost is basically Medi-Cal’s version of a deductible, or the amount that you agree to pay out of pocket toward medical expenses before Medi-Cal would take over and pay the remainder of expenses for the month.
- If your child is approved for a Medi-Cal plan with a Share of Cost that is too expensive for your family to afford, you can appeal the decision on the basis that the child does qualify for a deeming waiver by filing a discrimination complaint or requesting a hearing with the Department of Health Care Services.
Durable medical equipment (DME)
Unlike consumable medical supplies, durable medical equipment (DME) can withstand repeated uses over time. In order for Medi-Cal to consider covering your child’s DME, you must apply for prior authorization and prove that the equipment is medically necessary and prescribed by your child’s doctor.
Examples of DME include mobility aids like canes, gait trainers, and wheelchairs; assistive and augmentative communication (AAC) devices; bathroom equipment like rails, seats, and bath chairs; and respiratory equipment like CPAP machines, oxygen racks, and ventilators, to name a few.
Medi-Cal typically covers the lowest-cost equipment that meets a patient’s medical needs. For example, Medi-Cal would likely agree to cover the cost of a manual wheelchair for a child who has the ability to propel it, but they probably wouldn’t cover a motorized wheelchair for that child (unless a physician can show why it is medically necessary) since the lower-cost option, the manual wheelchair, would meet their medical needs.
As always, private insurance must pay its share of a DME purchase before Medi-Cal will agree to cover the rest. Make sure that the DME provider you choose contracts with both your private insurance and your Medi-Cal plan. Once private insurance pays its obligation, the DME provider will bill Medi-Cal for the remaining balance (up to the approved Medi-Cal rate for service). When a provider contracts with Medi-Cal, they are agreeing to accept the Medi-Cal contracted rate for the services or equipment they provide, so once Medi-Cal has paid its share for an item that is covered under Medi-Cal, the provider has been paid in full — they cannot bill you for any leftover balance for the covered item.
- There may be a remaining balance for items not covered by Medi-Cal, but this should be discussed prior to purchase. For example, if you purchase a wheelchair for your child and request a cup holder and decorative spokes for the wheels, Medi-Cal will pay for the cost of the wheelchair itself but not for the cup holder and spokes, as they are considered convenience and decorative modifications and are not medically necessary. You are responsible for paying the provider for any non-essential modifications made to the chair. However, the provider cannot bill you for the chair or medically necessary accessories even if the retail cost is more than the contracted Medi-Cal rate.
If your request for DME is denied, you can request a hearing with Medi-Cal to appeal the decision.
Home nursing/skilled nursing care
Home nursing or “skilled nursing” services are intended to provide children with disabilities under the age of 21 with skilled medical care so that they can continue living at home. Typical home nursing accommodations include Pediatric Day Health Care (PDHC) and Private Duty Nursing (PDN) services.
Medi-Cal may cover home nursing care for your child if their care team determines it is medically necessary for them to remain comfortably living at home. Medi-Cal will make an eligibility determination based on an assessment carried out by a Medi-Cal-contracted nursing agency. The nursing agency may ask you to fill out a HIPAA release form so that they can request information from your child’s physician.
If you don’t agree with Medi-Cal’s determination for your child, you can request a hearing to appeal the decision.
Housing and vehicle modifications
Housing and vehicle modifications allow people with disabilities to more comfortably get around their homes and the world at large. Modifications could be as simple as installing grab bars next to the toilet or as complex as constructing a wheelchair ramp leading to your front door.
Because of their variability and cost, any home and/or car modifications require prior authorization from Medi-Cal. Additionally, Medi-Cal may identify and authorize a less expensive or different modification than the one you originally requested; it is their policy to cover the lowest-cost option that fulfills a beneficiary’s medical needs, even if it’s not the modification you or your doctor specifically requested.
If Medi-Cal doesn’t approve your prior authorization or your request for a specific housing and/or vehicle modification on the basis of it not being the lowest-price option, you can request a hearing to appeal the decision.
In-Home Support Services (IHSS)
In-Home Supportive Services is a Medi-Cal program that can provide children with disabilities with much-needed assistance in the home. IHSS services are intended to support people with higher care needs in living safely at home in their community instead of in residential treatment centers. IHSS-sponsored care services could include in-home personal care services, diapering, meal preparation, protective supervision, accompaniment to medical appointments, and more. Read about what services are offered as well as how to apply.
In order to receive IHSS services, your child must be enrolled in Medi-Cal. IHSS hours are awarded when a child’s needs exceed those of a typically developing child of the same age. For example: IHSS is unlikely to approve toileting hours for a two-year-old child with disabilities who is not yet toilet-trained, but a ten-year-old child who requires diapers or toileting assistance would likely be authorized for hours in that category. Learn how to become a paid parent provider in our article on choosing IHSS providers.
If your child is denied IHSS services, you can request a hearing with Medi-Cal to appeal the decision. You can also appeal if you believe your child needs more IHSS hours than they were approved, but know that IHSS could increase OR decrease hours as a result of the appeal. For more, read our article How to Appeal If You Are Denied IHSS.
Medically necessary physical, occupational, and speech therapy
- Occupational therapy encompasses a wide range of treatments and interventions for both physical and neurological disabilities that might interrupt a child’s ability to go about their daily life.
- Physical therapy uses prescribed exercises and hands-on care to treat various injuries, disabilities, and other conditions that affect a child’s gross motor skills, or their ability to use their large muscles in the arms, legs, and torso.
- Speech therapy, also known as speech-language pathology, uses various therapeutic approaches and tools to treat communication/speech difficulties and disorders including motor dysfunction, fluency, apraxia, and dysarthria. A speech therapist can also train your child to use an AAC device, when appropriate.
Medi-Cal may cover occupational, physical, and speech therapy services if your child’s physician deems them medically necessary. You will need to obtain prior authorization first.
If Medi-Cal doesn’t approve a prior authorization, you can request a hearing to appeal the decision.
Neuropsychology services
Pediatric neuropsychology is a field within clinical psychology that assesses a child’s cognitive, behavioral, emotional, and social functions. Medi-Cal may cover neuropsychological testing if your child’s physician deems it medically necessary and obtains prior authorization. Testing is typically considered medically necessary if a child presents with noticeable mental deficits that could denote potential neuropsychological abnormalities (aside from learning disabilities).
If Medi-Cal doesn’t approve your request for neuropsychology services, you can request a hearing to appeal the decision.
Prescriptions
As of January 1, 2022, Medi-Cal covers prescriptions deemed medically necessary through its Medi-Cal Rx program. Many commonly prescribed medicines are pre-approved (find the list here) and will be covered by Medi-Cal without needing prior authorization. If your child’s medicine isn’t pre-approved, don’t worry: Medi-Cal may still cover it, but you will need to obtain prior authorization first. Medi-Cal may also cover certain over-the-counter medications if your child’s physician determines them medically necessary. Additionally, for over-the-counter medications, Medi-Cal won’t cover it unless it's processed as a prescription at a pharmacy that accepts Medi-Cal.
Some pre-approved medicines are only pre-approved to treat certain conditions. If your child needs a medication that is prescribed off-label — meaning, the medication is being used to treat a condition it wasn’t designed to treat — then Med-Cal will require prior authorization.
Some pre-approved medicines also have pre-approved supply limits attached to them. If your child needs more than the pre-approved limit, you will need to request prior authorization before Medi-Cal agrees to cover it. This most notably applies to controlled medications — if your child needs more than a 35-day supply of any controlled medication, Medi-Cal requires prior authorization.
If Medi-Cal doesn’t approve your prior authorization, you can request a hearing to appeal the decision.
Respite care
Respite care allows primary caretakers of children with disabilities to take much-needed breaks from caregiving. Respite care could take many forms but generally refers to a hired caregiver taking over child care tasks for a few hours a day, week, month, or as needed.
Children who are clients of Regional Center will receive their respite care through Regional Center. Children who are not eligible for Regional Center may still receive respite care through Medi-Cal if they are IHSS recipients: if a child’s parents or caregivers work full time and they have a non-parent IHSS provider, up to eight hours per week of their IHSS hours may be used for respite care while they are attending to other household needs.
Therapy programs
Though Medi-Cal typically only covers day programs for adult beneficiaries, your child may be able to obtain funding through other routes. Regional Center may cover funding for day care services if a client’s care and supervision needs exceed those of a non-disabled peer of the same age to the point that they cannot participate in typical (“generic”) community childcare resources like before-school and after-school programs. Hours are typically awarded during periods when a child is not in school, such as after school or during summer break. Regional Center may fund other programs as well, including early intervention therapies, social skills classes, behavioral intervention, respite care, and more. To learn about Regional Center programs and how to access them, read our article Regional Center 101.
Vision and dental
Vision and dental benefits are available to children with full-scope Medi-Cal benefits, according to the California Department of Health Care Services.
Medi-Cal Vision benefits include a routine eye exam and new eyeglasses once every 24 months. Medi-Cal will cover contact lens testing if the use of eyeglasses isn’t possible because of eye disease or a condition such as missing an ear. Low-vision testing can also be covered under Medi-Cal vision benefits if it's deemed medically necessary.
Medi-Cal Dental covers various dental services, including but not limited to diagnostic and preventative dental hygiene services like teeth cleanings and X-rays, emergency services for tooth pain, fillings, root canals, crowns, and orthodontics for qualifying children.
Resolve a dispute with Medi-Cal by filing a grievance
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor