Common Behavior Challenges in Children (and How to Approach Them)
Behavioral challenges can be confusing, overwhelming, and exhausting for parents and kids alike. Common challenges include tantrums, refusing to go to school, head banging, skin picking, flopping, refusal to engage in a task, biting, hitting and pushing, bullying other children, snatching toys, lying, and wandering off. Many of these are hard to understand and respond to when they’re happening, but trying to find the root cause and approach bigger prevention techniques may feel impossible.
“It's one of the hardest things because in the moment, a lot of times if a child is already dysregulated, there isn't a lot that you can do,” says Dr. Scott Akins, chief of developmental behavioral pediatrics UC Davis, Department of Pediatrics and medical director at the UC Davis MIND Institute. Every approach will have a different way of handling these behaviors, so we’ve shared a few of them below.
Tantrums
Tantrums may be one of the biggest challenges of parenting kids, especially kids with disabilities who don’t have the language to express their big emotions. Dr. David Stein, pediatric psychologist, explains that tantrums are a normal part of child development, unless they're happening all day, every day for hours on end. A tantrum a day or a couple of tantrums a day is not abnormal.
“The way that I view tantrums, which has some science behind it, is that a child has been holding it together all day long at school, or daycare, or whatever it is. And there's a lot of stress building up in their mind and their system and they just gotta let it out,” he explains. “So I've seen kids where they held it together all day with all their subjects and all their homework, and then mom put the chicken on the wrong spot on the plate, and now we're going to lose it and have a tantrum for 10 minutes. Is it that we need to have an intervention about where we put our chicken on our plate? No, it's that the child just had some stress built up in their system and they needed to let it out. So it's normal and it's okay, as long as it's not really extreme or violent or too much or too long. And there are some guidelines about that.”
What’s a mistake some parents make when it comes to tantrums? He tells us that when a child is having a big tantrum, trying to talk it out or ask why they’re having the tantrum is a big mistake. Parents need to let the tantrum pass and ride it out “because it's this big ball of emotion and energy that they need to get out. Once they get it out, then they can have more of a rational conversation. But in the middle of a tantrum, the front of your brain, which is where all the reasoning and logic live, is totally offline. We are thinking with the backs of our brains, our animal brains, and there is no logic, there's no reason, so it's pointless… So when a tantrum is happening, let them go. I try to check in every few minutes and say, ‘Do you need a hug? Do you need any water?’ So they know that we're there to support them but we're not going to try and talk them out of the tantrum because that's not going to work. And the tantrum is a normal healthy part of development, even though it's unpleasant.”
However, if your child is behaving aggressively or hurting themselves during tantrums, such as head-banging, there are some strategies you can use in the moment, and later to develop a plan for avoiding the behavior in future. Some of these strategies can include staying calm, limiting what you say, moving your child to a safer place or environment, using visual cues, removing harmful items and providing alternatives, redirecting your child to another activity, and praising your child. Read more about these strategies here (while this article is aimed at children with autism, many of the strategies are universal!).
Eloping
Many parents of children with disabilities, especially autism, find that their kids tend to wander away, whether that’s running off from home to play down the street, or leaving a classroom. This behavior is called elopement, or wandering, and is a serious safety concern. There is a high risk of getting lost or hurt, and if they can’t communicate who they are or where they live, it can quickly turn into a dangerous situation.
One of the most dangerous aspects of eloping is drowning. The National Autism Association says that accidental drowning accounts for 91% of deaths reported in children with ASD who are 14 years old and younger. For this reason, it is very important that children who elope are taught to swim, and adapted swim lessons should be funded as a safety concern, rather than access to recreation.
But why do kids wander? The National Autism Association explains, “Wandering/elopement is typically a form of communication, often occurring to get to something of interest or away from something bothersome, usually noise, commotion, fears/phobias, and demands. These impulses and incidents can increase with added anxiety and stress, especially if the individual has challenges with coping, calming, or regulating their emotions.”
Some of the primary reasons a child elopes include:
- They simply enjoy running or exploring
- They are going to a place they enjoy, such as a park
- They are trying to leave a situation that causes stress, school demands
- They are trying to escape uncomfortable sensory stimuli, such as loud noise
- They are heading to see something interesting to them, for example the local zoo if they love animals
Rose Griffin, speech language pathologist, Board Certified Behavior Analyst, and founder of ABA Speech, explains, “If the child is eloping, we want to see: are they eloping to go somewhere? So let's say a kid is trying to leave their house. Why are they leaving? Do they want to go outside to take a walk? Do they want to go to McDonald's? Whatever it is for the kid, it goes back to communication. Why is the kid just leaving? Do they want to go somewhere? Can they tell us that? Are they equipped to have a device or pictures, or are they talking to be able to discuss that?…. Think about the functional communication piece. Does she want to go see her friends? Well, you need to tell me that. And those are things that we all have to think about from a communication standpoint.”
She adds that then from a parenting standpoint, parents can have someone come in, such as a BCBA on your child's team, and have a home visit to figure out how parents can keep their child safe. For school, parents can request a 1:1 aide to their IEP if the child has a tendency to wander off at school.
Dr. Stein explains that eloping, as well as flopping, are signals from a child that something's wrong. He gives examples: “This class doesn't work for me, this time of day, this transition, whatever it may be, is not working. And therefore, I'm going to exhibit these behaviors.”
He continues, “So after the behavior has happened, it's really tough. If someone has already run away or flopped to the floor, it's really hard. The big thing is we can respond to the behavior without reacting. We can respond and go help that child get back to a safe place without getting really upset and worked up and reinforcing the behavior inadvertently. But really, what we have to do is look at what's going on before to trigger that behavior, and then what's happening after it to reinforce it.” He adds that that’s where a Functional Behavior Assessment and a positive behavior support plan come in — to get ahead of the behavior and intervene before it even occurs because we understand the nature of it.
Request a Functional Behavior Assessment (FBA)
Biting (and other sensory behaviors)
If your child is biting, there may be an underlying sensory issue at play. Sensory processing symptoms exist on a spectrum, and no one person experiences or responds to them in the same way. For example, a child may bristle or melt down in response to bright light, loud noises, or certain smells. Depending on the intensity of your child’s sensory challenges and co-occurring conditions, they could present with milder or more severe sensory-seeking and/or sensory-avoiding behaviors. A child with more severe sensory issues might react by hitting themselves, screaming, biting, or smearing feces. A well-designed sensory diet, which is a set of compensatory strategies and activities created by an occupational therapist to help a child better cope with sensory processing difficulties, can help alleviate that discomfort.
Dr. Marielly Mitchell, pediatric occupational therapist, reminds us that every behavior is a form of communication, even biting. The real question is what is your child trying to communicate?
School refusal
School refusal — also known as school phobia or school avoidance — describes a child’s regular refusal to go to school or stay at school. However, the child isn’t skipping school because they want to or because they just don’t feel like going; they’re doing it because school has become a place they just can’t cope with.
Step 1. Understand why
The first step is going to be to find out the why and understand the issue from your child’s point of view, and not be afraid to dig into the reasons why. Dr. Sally Burton-Hoyle, professor, ASD Area, and faculty advisor in the Department of Special Education College Supports Program at Eastern Michigan University, explains, “When kids don't want to do things they previously enjoyed, such as going to school, it should set alarms off with families. Professionals and families may ignore and feel the child needs to get used to it.”
She explains, “Families often state that their child was really happy last year in elementary, and now they're in middle school, and they just don't seem happy. The easiest way [for a school] to get a parent off their back is to say, ‘Everything's fine, we've had no reports.’ But families should dig in and trust their instincts and figure out the why because there is always a reason. Sometimes bad things are happening to the child so families should look at behavioral changes. What if your child becomes afraid of something they’ve never been afraid of? This is when parents need to pay attention to any changes in sleep, affect, appetite or emotions. They need to believe in their child, and in themselves. Parents must investigate until they are satisfied that their child is safe and supported.”
Dr. Stein agrees, telling us that it’s important to find out what's driving the school refusal, and that it could be more than one thing. “Let's look at where they are cognitively. Let's look at where they are academically. Let's look at where they are emotionally and socially. And is their program a fit? Are they avoiding the school because it's not appropriate or it's not the right program? Kids act out when they don't have other choices. Or, and this is not a mutually exclusive type of thing, is there some anxiety, some depression, some other issue going on with the child that's driving that behavior? And again, it could be both, right? It could be that your program is not a fit and you're depressed. So we have to address both. We have to look at: is there a match between where they are developmentally and what they're being asked to do? And then is there something else at play like a mood disorder or anxiety?”
Step 2. Develop strategies
Dr. Burton-Hoyle adds that parents can request a Functional Behavioral Assessment (FBA) that examines a child’s whole life at school, not just a snapshot of them during lunch. For example, where they're going at school, what environments they're in, how they’re communicating their behavior, and if there’s something they don’t like at school. An FBA may show where your child may be having trouble and if they need more, or different, supports at school. Some strategies may involve access to a quiet or private space that the child may go to if they feel anxious or upset; access to communication devices or visuals to communicate to teachers or staff if they need a break or need to ask for help; access to sensory toys that may help ease anxiety, etc.
Parents may ask to sit in on any interventions or therapies a child is in to see how their child is responding and enjoying them. Perhaps a child doesn’t like a certain provider or a certain intervention. She says, “If I were a parent, I would want to see instructional videos on each of the therapies and time to observe it in real time. In the situation of an IEP, where a kid is transitioning to a different setting, schools normally allow initial parent visits for observation. Parents should also observe current setting to see if their child is valued. Are professionals, teachers, and therapists presuming competence in them? If you're presuming competence in a child during your therapy, that child is going to flourish. When children have positive relationships with their school professionals, then they're going to want to get on the bus and go to school.”
See our full article on school refusal for a deeper dive. For other tips on motivating kids to go to school with optimism (not to mention the dreaded task of homework and other non-preferred activities) read our article Motivational Strategies for Going Back to School.
Address my child's school refusal or avoidance
Rethinking stimming
Stimming is shorthand for repetitive, self-stimulatory behaviors. While stimming is commonly associated with autism, it can also occur in typically developing kids, kids with ADHD, and kids with many other co-occurring diagnoses. Stimming can take many forms, from hand-flapping to squealing to finger-flicking to head-banging. As a term, “stimming” has been reclaimed by people in the autistic community to describe self-stimulatory behaviors (sometimes also called “autistic stereotypy”). But some approaches to stimming, such as ABA, have historically been compliance-based, teaching kids to have “quiet hands” to help them regulate and/or cease self-stimulatory behaviors.
Research has shown that “stims are a response to either sensory overload (such as a noisy room) or overpowering thoughts… stimming soothes these intense feelings, helping them regain a sense of control.” Stimming also sometimes helps kids communicate their moods, whether that's joy, anxiety, overwhelm, or boredom. We know that stimming is an essential calming strategy for many kids, but when it really gets in the way and becomes a behavior, what can parents do?
Dr. Burton-Hoyle tells us that stimming begins as a child trying to meet a need. If we don't pay attention to what that need is, we might tell them not to engage in stimming or try to make them compliant. So figuring out what it means, whether it’s involuntary or based on a need, is very important.
Griffin adds that stimming should be approached on an individual basis: “I would never stop somebody from stimming if it was something that made them feel good. If it's something that's completely unsafe in the environment, then I think that we have to look at it that way. Like, is this student unsafe? But if it's not a barrier to their learning, then I think that we just kind of let it be. And then we enrich the student’s environment to get them involved in lots of different activities,” to meet their sensory needs, such as speech therapy, using swings, being more active on the playground or the gym, etc., “and just trying to embed all those things across our students' day.”
If stimming is a barrier to learning, or self-injurious, it’s important to understand that the goal shouldn’t be to stop the behavior from occurring as the child will likely engage in another form of stimming that could be much worse. Instead, offer a replacement behavior for the stim behavior. As Stanley Greenspan, author of Engaging Autism and developer of the Floortime method, explains in this article from The Child Mind Institute, “The overall principle is to offer the child experiences that produce the same sort of sensations as the self-stimulatory activity but lead up the developmental ladder of regulation, engagement, and interaction.” Read more about stimming in our article Rethinking Stimming: Perspective.
Toilet training
The process of toilet-training can be frustrating for any parent. While a typically developing child is usually toilet-trained by the age of three or four, an “average” age for kids with disabilities doesn’t really exist. It’s important to know that the reasons a child may have trouble with toilet training can be physical or behavioral (or both) — and knowing which it is can help in the creation of strategies and interventions. For example, kids with spinal cord abnormalities or irregularities are going to have urinary issues. Kids with cerebral palsy may require an adaptive seat, as balance and sitting in an appropriate position can be difficult. But once any medical complications have been addressed and/or ruled out, it’s time to tackle the behavioral causes that can make toilet-training hard to navigate. And this can simply mean that a child doesn’t understand the behavior.
As Dr. Burton-Hoyle explains, she’s had experiences with ABA techs who have said a child was non-compliant in toileting. But she wants us to think beyond the behavior to what else could be going on. For example, the child may not know how to do it, or understand the process well, or even understand the basic bodily feeling. “Because if we look at interoception, that’s the notion that people who are neurodivergent probably don't have a good idea of how they're feeling. So if you don't know that you're hungry or that you're thirsty, you're not going to go get a drink of water.”
The same applies to toilet training. Does your child know to recognize that they need to go to the bathroom? Does your child know the difference between a wet or soiled diaper or underwear versus a dry one? If the answer is no, start showing them what “wet” feels like on their skin. And this mentality can also apply to some of the most challenging behaviors, such as smearing of feces or even a curiosity for some children to taste it — maybe they haven’t been told in a way that makes sense to them that that’s not something we play with.
Read more about toilet training, including toilet-training difficulties, how to start, and what steps to take if we’re feeling stuck in our article here.
Help my child with toilet training
Pathological demand avoidance (PDA)
All children, from time to time, avoid and outright refuse to do things they’re asked. Often, this can be how they assert independence, preferences, or needs. But sometimes, this avoidance can be extreme.
Pathological demand avoidance (PDA) is a term used to describe a personality and behavioral traits, often exhibited by people with autism, who tend to refuse to cooperate with others’ requests. Those with PDA “use social strategies to avoid demands and to mask anxiety or underlying processing and communication issues.” Other research shows that “avoidant behaviors in children described as having PDA are often triggered by phobias, novelty, and uncertainty.”
Dr. Burton-Hoyle tells us that PDA is a high degree of resistance, but ultimately, it’s not a diagnosis and it’s not in the DSM (as of now). Many professionals also believe that the term pathologizes a person’s preferences and autonomy without looking at the reason behind the behavior. For example, which requests or demands is a child refusing, and why? Often, kids with autism may not have the same motivations as typical children to fit in or follow rules. It can also be a form of self-advocacy.
The PDA label on its own also doesn’t qualify a child for special education. “I really feel that families need to think about what would my child qualify for within special education. If it's not a special education issue, families need to figure out the supports they may need in order to be successful,” Dr. Burton-Hoyle says.
As with other severe behaviors, experts recommend that parents find ways to understand the why, as well find ways to support and motivate kids in developing flexible thinking and appropriate adaptive skills. For example, building in strengths and preferences into the daily routines, such as a specific activity may change the child's day and lead to positive outcomes. As Dr. Burton-Hoyle says, it’s important to be creative and look for strengths in children.
For more information, see our full article Pathological Demand Avoidance (PDA) 101.
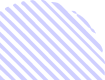
A few tips for supporting kids (and yourself) through behavior challenges
You can use a multidisciplinary approach
When dealing with these common behavioral challenges, especially ones that are more severe such as self-injurious behavior, Dr. Burton-Hoyle recommends that parents use a multidisciplinary approach: “I think families, when it's severe, need to think beyond just the behavior, the outward behavior that they're seeing, and look at, ‘What else could we do?’”
Dr. Stein also emphasizes looking at what drives the behavior in a larger way, emphasizing understanding behavior, understanding relationships, and understanding the brain.
Honor your child’s voice
Positive interventions don’t have to happen at school; they can also work as an approach relationally between parents and children. Dr. Burton-Hoyle explains that parents are the best observers of their children, and one way parents can positively approach behavior is to presume competence. She says, “I think parents need to presume competence in their children. The one actionable way parents do that is to talk to the child directly and not around them and insist that other people do that as well.”
This includes therapists, providers, and teachers. Parents can inform teachers of this and that they do not want staff to talk about the child in their presence. For example, she explains, “You can say to the child, ‘Johnny, you seem to be having a really difficult day. Do you mind if Miss Jones tells us what happened in our class?’ And that might not seem like an important thing, but it is huge. I've heard it from way too many individuals that when people talk about them, or around them, that it's like somebody's kicked them in the stomach.”
She also adds that parents need to truly understand that behavior is legitimate communication. Parents can advocate for their children by telling a therapist or provider, “By my child's behavior, I think he's really telling us that he's not happy with how such-and-such is going.” This is a way to honor a child’s voice and instill in them that you believe in them.
Learn about behavior
Another tip is to invest in learning as much as you can about your child’s behavior, whether that’s through watching YouTube videos, reading books, or getting parent training. For kids with autism, Dr. Akins recommends “Help is in Your Hands” from The MIND Institute, which offers 16 web-based video modules to help parents with intervention practices to their everyday routines at home, specifically around behavior. He also recommends the MIND Institute’s free ADEPT (Autism Distance Education Parent Training) Interactive Learning, which is “an original MIND Institute/CEDD 10-lesson interactive, self-paced, online learning module providing parents with tools and training to more effectively teach their child with autism and other related neurodevelopmental disabilities functional skills using applied behavior analysis (ABA) techniques.” It covers structured individual seminars around managing challenging behaviors and facilitating communication.
“For me, those can be so helpful because you can watch them at 9:00 at night after the kids have gone to bed,” he says. “And when many of us are worrying, or you're looking online for something and going down a rabbit hole where you're wondering if you should be doing some kind of a vitamin treatment, these are evidence-based treatments that really get at the heart of the challenge that most people are having around behavior, and will help you learn some tools, tricks, and strategies that you can use.”
Dr. Stein’s book Supporting Positive Behavior in Teens and Children with Down Syndrome is also a great place to learn about using the functions of behavior in a way that emphasizes the relationship between parent and child. To learn more about Collaborative and Proactive Solutions, there are step-by-step video guides at Lives in the Balance, provided by Dr. Ross Greene, author of The Explosive Child, Lost at School, Lost and Found, and Raising Human Beings.
Visual schedules
Dr. Burton-Hoyle adds that helping kids self-manage and have daily schedules can also help with the feelings of overwhelm that may result in severe behavior and PDA. This means that kids know what their ‘now’ and their ‘next’ are. “When families begin to help their kids schedule their days, they learn what things are helpful and things that aren‘t” when it comes to managing and decreasing certain behavior or triggers to those behaviors.
She recommends visual supports as opposed to auditory because auditory processing is often the weakest link when a child has any kind of neurological difference. This can be in the form of a visual schedule, which can help kids with following a routine, transition between activities, develop new skills, and be more independent when completing daily tasks. Visual schedules can consist of photographs, videos, line drawings, symbols, text, or another visual format that is used to show the user what they are expected to do. These tasks are then arranged in the order they are to be completed. This provides the child with predictability and expectations.
One practical tip she offers parents is to have a central communication system in the house, such as the refrigerator, which can be used to communicate expectations and prime children. “So on the refrigerator, have pictures or words of, ‘This is Saturday, we're going to do this or this, and you have a choice of this…’ So if we teach people how to kind of organize their day, and include what they need to do, and want to do, then there's going to be more balance and they're going to feel like they're heard. I cannot begin to tell you how meaningful that is because then the child is going to feel like they have some control over their life.”
Reinforcements and social rewards
If getting your child to participate in non-preferred activities is incredibly challenging, you can use a variety of techniques at home. For example, reinforcement and motivation is an important part of ABA therapy. There are many ways to practice this at home, including using a token system, where the child earns access to something they’ve agreed on beforehand with the family, even rewards apps.
Dr. Stein gives a great tip when it comes to reinforcements: the best reward for most kids is something social! For example, playing a game with a parent, reading together, etc. “Time and social interaction is the best because number one, it's the most powerful reinforcer… Stickers or bracelets, they lose their appeal, right? How many times can you get a new junky bracelet that's going to turn your arm green? Food and other things like that are not as good of a motivator. But attention from another human being that you love never really gets old. So yes, I prefer to do social rewards.”
There are also a wealth of online materials for behavior support at home put together by therapists, artists, parents, app-makers, cookie-bakers, and all-around creative people that offer exercises, videos, and fun activities across a variety of platforms. Check out our top 5 resources to help incorporate behavioral therapy into your daily routine, including a learning tool that helps children complete daily routines while understanding and controlling their feelings and improving waiting skills.
Dr. Akins talks us through one of his approaches for parents, where he uses zones of regulation to help with dysregulation, especially during temper tantrums:
Invest in parent coaching
With any therapy or intervention, working with providers to create strategies you can use at home is vital to creating consistency across settings. It’s not enough to just focus on behavior at school, or at home, or at the park. If we’re exploring a whole-child approach to managing and exploring behavior, parents need to incorporate strategies that cover all areas of a child’s life.
If you’re in ABA, for example, Dr. Akins says it's important that parents get the caregiver coaching component where you meet at least twice a month for an hour or two with the BCBA and work on the part for you at home. “It’s great that your child is going into therapy and they're learning communication skills and imitation and new puzzles — that's really important. But if you're still struggling to get them to bed every single night, or if the bathroom routine for teeth brushing is a disaster and a huge meltdown every single night, you should get caregiver coaching from your ABA therapists around that. They should help you have very clear strategies about what to use, whether it's just a visual schedule or an incentive schedule or a first-then board, whatever it might be that they're trying in a structured way.”
He adds that this also helps you gather information and data about your child about, for example, how long a tantrum lasts from one day to the next, and what’s working or not working so you can get clear guidance. “I think that's the part that sometimes doesn't happen for families, and so the therapy is less meaningful for them because it's not helping with family function,” he tells us.
Communicate with providers
Behavioral challenges are tough on any parent. Take a moment to breathe and know that there are many options and avenues to support you and your family.
Whichever therapy you decide to explore, Griffin tells us that there should always be ongoing communication and support from your providers. “There shouldn't be anything taking place that you don't feel comfortable with or you're not sure why it's happening. And so I would just say, make sure that ongoing communication is there and that you as the parent are able to go in and see, well, what does this therapy actually look like? And if you have questions, can the provider answer them? If you have questions, what is the reaction of the provider? They shouldn't be defensive. It should just be, ‘This is why we're doing this, and this is the reason.’ And so having that positive rapport and making sure your providers are active listening and taking your concerns to heart, I think those things are all really important because then you as the parent will feel more comfortable to say, ‘I don't really feel comfortable with this,’ or ‘I'm not sure why you're doing that.’ And then getting the rationale for that, especially for very young students.”
Join for free
Save your favorite resources and access a custom Roadmap.
Get StartedAuthor